Too bad. Ulcers coupled with scars are very bad. Scars, especially on scalp, are quite sensitive. They need close monitoring. Due to negligence and poor management scars can deteriorate. This causes complications as severe as Marjolin’s ulcer. Marjolin’s ulcer arises from chronic wounds as malignant tumors. Likewise, burn scars and pressure sores are open wounds which often give rise to Marjolin’s ulcer.
This is a case of 58-year-old man. He experienced an injury during bear mauling roughly 50 years back, which means his childhood. The injury healed and produced a scar. Above all, it is necessary to know that scars also require prompt management. Otherwise they go through alternate sequence of healing and deterioration. Soon a chronic scalp scar forms due to deteriorating scar.The size of ulcer increased with each passing day. The appearance of scar became quite unpleasant. In this case, A cauliflower-like granulomatous mass had produced in the center. Blood and foul-smelling serosanguinous discharge accompanied the increase in size and white-colored granulomatous formation.
This is a case of Marjolin’s ulcer. It is a very rare complication. It often occurs due to trauma or negligence towards non-healing scars. Furthermore, it is quite rare and aggressive development which is often epidermoid carcinoma in nature. Scalp scars and scalp necrosis are rare but equally difficult to manage.
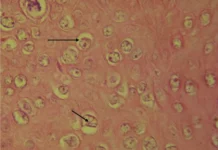
Hemorrhagic and necrotic ulcer
The patient belonged to a below-average locality. Due to poverty and negligence the worsening condition of non-healing scar could not be prioritized. Upon examination the patient was conscious and had stable vital signs. Surprisingly the patient didn’t report a fungating mass of 10 cm x 12 cm x 5 cm which extended up to the occipital region. The mass appeared pale white with breaks and cracks exposing hemorrhage and necrosis. The patient must be under extreme discomfort. Living with a bleeding and foul-smelling necrotic mass on head is not least bit easy.
Cytology and CT Scans
Further investigation was necessary to understand the nature of necrotic and hemorrhagic mass. The scrape cytology revealed squamous cell carcinoma. The right occipital and posterior triangle lymph nodes had undergone inflammation.
Upon fine needle aspiration features of inflammation and reactive hyperplasia were found. CT scan showed right occipital extra-calvarial isodense lesion with underlying bone erosion and meningeal thickening. The scans and cytology tests reflected involvement of brain tissue, skull and meninges. Apparently, this case demanded scalp remodeling which urged to be a case of plastic surgeon. However, involvement of neurological structures categorized it under the interest of neurosurgery.
Removal of invasive ulcer and Remodeling of skull
Neurosurgeons and plastic surgeons mutually agreed to conduct urgent surgery to remove invasive ulcer and remodel skull. In the beginning of surgery, it was necessary to mark vascular musculature using Doppler’s ultrasound. The position of patient on operating table was prone position. Surgeons removed the lesion by a margin of only 2 cm from the skin. The structures lying underneath were clearly visible after removing the ulcerated lesion. Marjolin’s ulcer had damaged the bone, dura matter and tissue beneath. Now surgeons had to repair dura matter, concerned brain tissue and bone. G-dura patch repaired the damaged dura matter. However, surgeons preferred removing abnormal cortical brain tissue. Local rotation flap, which is based on left occipital artery, closed the defected scalp. Lastly, skin graft repaired the secondary graft.
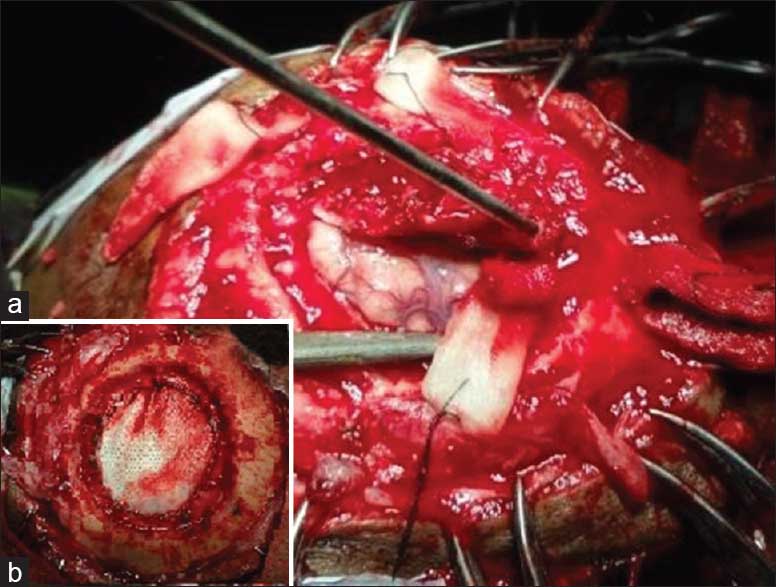
The patient had gone through immense suffering. However, he was equally lucky to achieve 100% flap survival. He was discharged a week later.