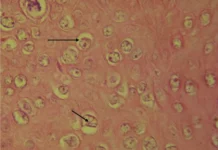
The image attached above is of a rare (5.5 to 7.9 per million live births) congenital anomaly in which the thoracic cavity fails to enclose the heart due to defective fusion of the chest wall, resulting in a partial or complete displacement of the heart outside the thorax. This is called Ectopia Cordis.
The case in the discussion here is of a 15 hours old, full-term male baby, weighing 2.25 kgs, and a product of non-consanguineous marriage. The baby was delivered vaginally with an uneventful antenatal and intrapartum period. Postnatally, the baby was brought with dyspnea and an externally pulsating heart over the anterior chest wall.
On examination following vitals were recorded:
Heart rate – 150/min
Respiratory rate – 76/min
SpO2 – 88%
Physical examination revealed peripheral cyanosis and a bifid sternum with two ridges of sternum being 5cm apart. Upon examining the eviscerated heart, it was found to be devoid of the pericardium.
It is important to look for other abdominal wall defects and intracardiac defects in neonates who are born with Ectopia Cordis as 80% of the cases are observed to be associated with intracardiac defects.
Ectopia Cordis, yet, has no known aetiology, though rupture of the chorion and amniotic band syndrome are being studied in depth as the potential causes. There is a slight male predilection but there is no evidence of increased chances in the siblings of the affected child. It has been classified:
1. Into four based on position:
Cervical (least common)
Thoracic (most common)
Thoracoabdominal Abdominal
2. According to its overlying covering:
No covering
Covered by serous membrane or pericardium.
Skin covered
3. According to associations:
Isolated Ectopia Cordis
Associated with other abdominal defects (for eg omphalocele)
Associated with abdominal defects and intracardiac anomalies
Ultrasonography readily diagnosis it in the antenatal period, usually during the first trimester i.e. as early as 10th week of gestation. When prenatal ultrasound is not performed, as in the case being discussed here, then the diagnosis is obvious right after the birth on the grounds of physical appearance and examination.
Unfortunately, Ectopia Cordis carries the burden of a high mortality rate, with only 10% of cases surviving. Even for the survivors, life isn’t a bed of roses. Extensive and complicated surgical procedures followed by specialised lifelong medical care becomes the part and parcel of their lives. Till date, no in utero treatment options are available.
Postnatally, immediate resuscitation and covering of the heart (and other eviscerated structures) with a sterile saline gauze are the first few steps. Emergency surgery is required to place the heart back in the thoracic cavity followed by surgeries to reconstruct the sternum for the protection of the heart. Not forgetting to mention here the other associated anomalies and defects requiring surgical corrections. The neonate in the discussion here resuscitated and kept in an incubator. Parenteral antibiotics and supportive treatment were started. Despite management, respiratory distress progressed enough to warrant mechanical ventilation. Neither ventilator nor ionotropic drugs were successful in improving respiration and cardiac activity, respectively. Unfortunately, the baby succumbed to death.
References:
Shad J, Budhwani K, Biswas R. Thoracic ectopia cordis. BMJ Case Rep. 2012;2012:bcr1120115241. Published 2012 Sep 30. DOI:10.1136/bcr.11.2011.5241
Retrieved from Children’s Hospital Colorado