As many as 5 million people in the United States live with Alzheimer’s disease (Mathews et al., 2019). The disease initiates with a range of symptoms including memory loss and confusion and progresses to difficulty with speech, thinking and orientation. Currently, the exact cause of the disease remains unknown and there is no cure for the disease.
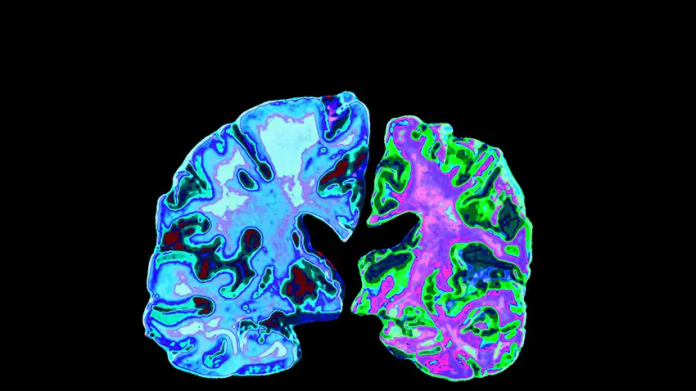
However, scientists have discovered sticky clumps of protein in the brain of people who died of Alzheimer’s called beta-amyloid. The protein has played a pivotal role in research related to the disease, to date. But, unfortunately, trials of drugs targetting beta-amyloid have been unsuccessful. Scientists believe that this is because the treatment started too late. The progress of the disease starts many years before the disease is diagnosed. The disease progression is generally at its last few stages when patients join clinical trails, deeming it too late to help the patients.
The critical window
The early stages of the disease are a critical window in the field of research. To find out what was happening in the brain before development of the disease, researchers began looking at earlier stages of cognitive decline. Also known as mild cognitive impairment, symptoms include losing things more than usual or forgetting names of items. Although, this is not always the case, these are signs that show at very early stages of the disease.
Neuronal death – a key process underlying Alzheimer’s disease
In the current research, scientists discovered neuronal death in mouse models, as well as in people with Alzheimer’s disease and mild cognitive impairment. Researchers measured how many neurons died using a protein the dying neurons release, called HMGB1. The study was carried out on 26 people with MCI and 73 people with Alzheimer’s disease. In addition, scientists also detected dying neurons at different stages of the disease, using a new biomarker called pSer46-MARCKS.
According to Hikari Tanaka, the lead author of the study,
“Neuronal death is obviously very important in the development of Alzheimer’s but is notoriously difficult to detect in real time because dying cells cannot be stained using chemical or immunohistological methods.”
Researchers were surprised to find that the neurons died much earlier than expected. Moreover, compared to the study participants with Alzheimer’s disease, the neurons died much sooner in participants in mild cognitive impairment. During the study, it was also discovered that the protein called YAP was responsible for the early death of neurons. In addition, previous studies (Xu et a;., 2018) have found that there is a significant link between YAP and Alzheimer’s disease. What’s more, researchers found the missing YAP trapped inside the clumps of beta-amyloid, that has been well-known to be associated with Alzheimer’s disease.
What does this mean for Alzheimer’s patients?
Researchers believe that their findings could lead to new treatment for the disease. New findings suggest that the YAP protein might actually be responsible for causing neuronal death.
“By showing that neuronal [death] is YAP-dependent and begins prior to the onset of most symptoms, we predict that novel Alzheimer’s disease therapies will be developed,” says Okazawa.
References
Matthews, K. A., Xu, W., Gaglioti, A. H., Holt, J. B., Croft, J. B., Mack, D., & McGuire, L. C. (2019). Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged≥ 65 years. Alzheimer’s & Dementia, 15(1), 17-24.
Xu, M., Zhang, D. F., Luo, R., Wu, Y., Zhou, H., Kong, L. L., … & Yao, Y. G. (2018). A systematic integrated analysis of brain expression profiles reveals YAP1 and other prioritized hub genes as important upstream regulators in Alzheimer’s disease. Alzheimer’s & Dementia, 14(2), 215-229.