Case of recurrent syncope in patient with amyloid cardiomyopathy.
A 63-year-old Caucasian female patient presented to the emergency with complaints of recurrent and progressive episodes of syncope which caused her to become bed-bound. The syncopal episodes began a year ago, triggered by positional changes and light-headedness. However, she had no gastrointestinal complaints, abnormal movements, tongue biting, urinary or bowel incontinence. She returned to the baseline after a few seconds of these episodes. Doctors diagnosed the patient with amyloid cardiomyopathy.
She also complained of unintentional weight loss while she was unwell. Doctors earlier advised tests including complete blood count, thyroid function tests, ACTH, electrocardiogram (EKG), echocardiogram, electroencephalogram and magnetic resonance imaging of the brain, computed tomography of the abdomen, upper endoscopy, and colonoscopy, all of which were unremarkable.
The patient’s past medical history was significant for Hurthle cell carcinoma of the thyroid gland.
She was diagnosed with Hurthle cell carcinoma 4 years ago for which she underwent thyroidectomy with an uneventful recovery. Physical examination showed cachexia with a supine blood pressure of 127/72 mmHg, heart rate 79 beats per minute, blood pressure 93/60 mmHg, heart rate 91 beats per minute. Whereas her sitting blood pressure measured 93/60 mm Hg, heart rate 91 beats per minute and standing blood pressure 73/42 mmHg and heart rate 97 beats per minute.
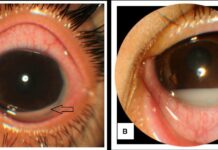
The patient’s oral examination was consistent with a moist mucosa and macroglosia. Examination showed clear lungs with distant heart sounds. No signs of organomegaly or peripheral oedema were evident. In addition, there were no skin bruises or periorbital purpura evident with an unremarkable neurological examination. Initial laboratory test results were also normal.
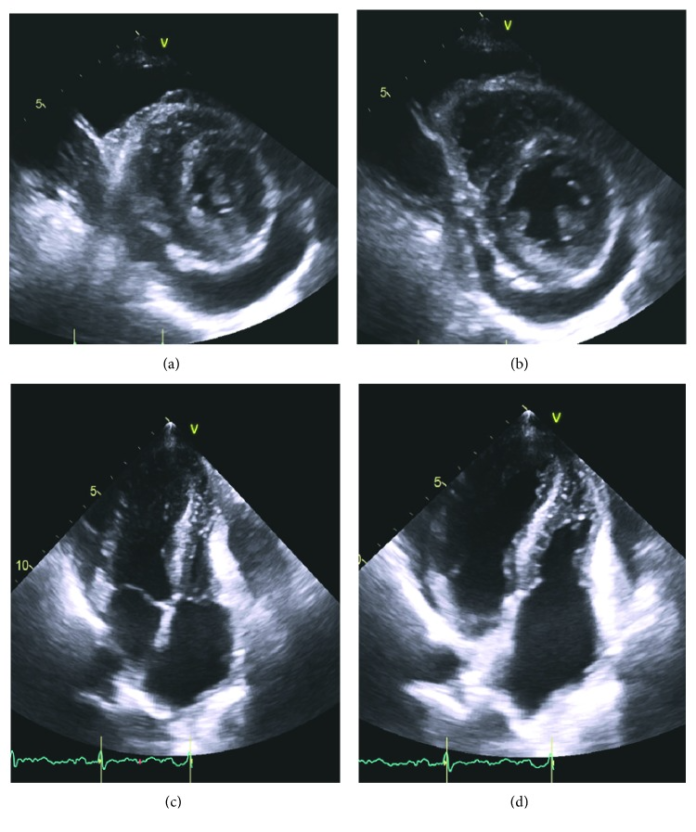
Doctors further advised an EKG which was consistent with sinus rhythm, low voltage in majority leads and left atrial enlargement. The patient’s trasnthoracic echocardiogram demonstrated large pericardial effusion, 73% left ventricular ejection fraction, grade I diastolic dysfunction, left ventricular hypertrophy, abnormal longitudinal contraction and speckled appearance of the myocardium. The findings led to the diagnosis of amyloid cardiomyopathy. Bone marrow biopsy further showed deposits of congo red positive amyloid and 5% atypical plasma cells with lambda restriction.
The mass spectrometry was suggestive of lamba-type cardiomyopathy.
The diagnosis was confirmed with cardiac magnetic resonance which showed suboptimal myocardial nulling. Whereas patchy focal late gadolinium enhancement affected the percardium and atrial walls in addition to a large percardial effusion and pleural effusion.
Treatment included a multidisciplinary approach including palliative care, cardiology, haematology/oncology and internal medicine. The patient choose to undergo an aggressive management approach with chemotherapy. However, the patient’s BP did not improve despite treatment. And her levels of lambda FLC increased progressively. Doctors advised palliative care because of her poor response to chemotherapy and overall poor prognosis. Unfortunately, the patient died two months after therapy was discontinued because of cariogenic shock.
References
Recurrent Syncope, a Clue in Amyloid Cardiomyopathy https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5829326/