Ophthalmic manifestation in patient with acute lymphocytic leukemia
This article describes the case of a 5-year-old boy who presented with a 3 day history of watering in his left eye. The child was currently under treatment for pre B-cell acute lymphoblastic leukaemia (ALL). Earlier the boy presented with a 2 weeks’ history of fever and doctors diagnosed him with ALL. Tests were significant for hepatosplenomegaly with thrombocytopenia. Whereas bone marrow studies and cerebrospinal fluid (CSF) analysis were conclusive of ALL with involvement of the central nervous system. He later developed uveitis with hypopyon, an ophthalmic manifestation of ALL.
After the diagnosis, doctors prescribed the patient weekly intrathecal doses of methotrexate. The treatment was based on regimen A (three drug induction) of UKALL 2003 protocol. At the end of the treatment investigations were consistent disease remission, however, with minimal residual disease, posing as a significant risk.
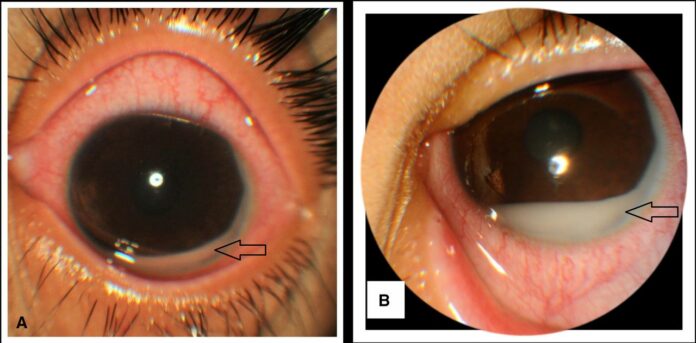
When the 5-year-old presented to the hospital, the delayed intensification phase had just completed and doctors had started him on a maintenance cycle treatment. Ophthalmologic examination showed a visual acuity of 20/20 in the right eye and in the left eye 20/200. An examination of the anterior segment showed circum-corneal congestion in the left eye. In addition, the anterior chamber revealed a white hypopyon measuring 2 mm.
A hypopyon is a medical condition with accumulation of inflammatory cells in the anterior chamber of the eye.
The cells include different types of neoplastic cells, macrophages, erythrocytes and leukocytes. The condition is generally accompanied with redness of the conjunctiva and underlying episclera. Anterior uveitis with hypopyon in the left eye was a remarkable feature for relapse on ALL in the child. Ophthalmic manifestations of leukemia can occur because of several reasons including direct infiltration of ocular tissues, hematologocal abnormalities and neuro-ophthalmic signs. acquiring aggressive local and systemic therapy.
Further examination showed that the pupil was meiotic, whereas the pupillary reaction was sluggish. There were also signs of lenticular opacity in the posterior subcapsular region and the intraoccular pressure was raised to 28 mm Hg. Doctors also referred him for an ultrasound which showed choroidal thickening and exudative retinal detachment. However, an analysis of the cerebrospinal fluid and bone marrow aspiration did not show a presence of leukaemic cells. Paracentesis of the anterior chamber showed atypical lymphoid cells consistent with leukaemic infiltration.
Treatment included reinduction treatment as per the protocol of ALL R3, following ocular and cranial radiotherapy. Further including a subsequent bone marrow transplant. Unfortunately the boy passed away a few months after the relapse was diagnosed.
References
Masquerade uveitis with hypopyon as a solitary feature of relapsed leukaemia in a child https://casereports.bmj.com/content/14/5/e240485#ref-6



