Psoas abscess: Introduction
Psoas abscess refers to the collection of pus within the muscle known as iliopsoas, present in the anterior compartment of the leg. Despite its rare presentation in the previous years, the incidence of such cases has risen significantly in recent times. This can be attributed to the availability and improvement in the use of diagnostic modalities such as CT scans and Ultrasound. Doctors may send other investigations such as full blood count, erythrocyte sedimentation rate, gram staining and creatine kinase to reach a definitive diagnosis.
There may be two causes of this abscess, primary and secondary. The primary cause refers to an unknown aetiology, whereas the secondary cause can be due to an underlying infection or direct inoculation with a contaminated object, like surgical instruments.
The most common infection that is responsible for this abscess is known as Staphylococcus aureus. Although, other rare organisms may also cause it.
This abscess presents with various symptoms including an abnormal gait, fever and lower back pain. Despite the overt specificity of the symptoms, doctors may fail to diagnose it at an early stage due to the similarity of symptoms with conditions like osteomyelitis, bursitis, sciatica, muscle strain and paraspinal abscess.
Doctors treat this condition depending on the underlying aetiology. The most common way to manage is by draining the abscess through radiological assistance. Additionally, doctors give the patients empirical antibiotics while they sent the aspirated fluid for culture. Once the doctors receive the culture report and the causative agent is identified, they may alter the antibiotic regimen and dosage.
This case highlights the formation of a psoas abscess secondary to tuberculosis, which has an incidence of 1%. Such cases are a diagnostic challenge due to nonspecific symptoms.
Case presentation: Psoas Abscess
A 38-year-old Syrian woman presented with lower back pain that began 4 months back and radiated to the right posterior thigh and right groin. Additionally, she complained of a tingling sensation and redness over the affected thigh. The pain was persistent and was not exacerbated by changes in posture or position. Therefore, doctors administered intramuscular dexamethasone to relieve the patient’s pain.
Examination and Investigations
On examination, the doctors found tenderness over the right paraspinal muscles along with the limited hip movement of the affected thigh.
The doctors sent some baseline investigations, which were normal. They also sent a Human immunodeficiency virus (HIV) test and QuantiFERON TB test. Both came out negative.
Radiological Imaging
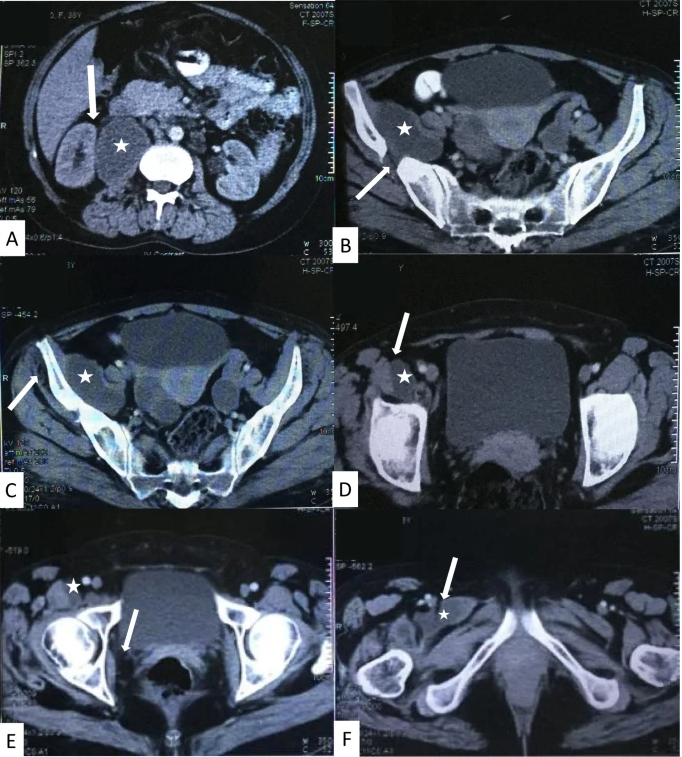
In order to reach a definitive diagnosis, the doctors ordered certain radiological imaging. The pelvic X-ray revealed necrosis in the iliac bone, despite there being no history of trauma. The Abdominal CT scan revealed displacement of the right hip secondary to the psoas abscess. Furthermore, it revealed the extension of the psoas abscess to other muscles. The muscles affected were the right femur adductor muscles, right obturator muscle, right piriformis muscle, and right gluteal muscles. The Chest CT revealed a nodule in the lower right lung lobe. Moreover, the MRI scan reported osteomyelitis of the right hip joint.
All the examination and investigation findings could not lead the doctors to a confirmatory diagnosis. Therefore, they performed a CT-guided biopsy of the abscess present in the right psoas muscle. They aspirated the fluid in this abscess and sent it for testing to the lab. The fluid was positive for leukocytes and the epithelioid histiocytic cells which suggested a preliminary diagnosis of tuberculosis. Although Ziehl–Nielsen’s staining and TB culture turned out to be negative. No other bacterial specie was isolated in the sample as well.
To confirm the diagnosis of tuberculosis, the doctors took a sample of the psoas abscess lesion and sent it to the laboratory for assessment. This came out positive for granulomatous TB.
Thus, after a series of various tests and inconclusive evidence for the presence of Mycobacterium Tuberculosis in the psoas abscess. A sample of the lesion eventually confirmed the diagnosis. The doctors began treatment for the eradication of the bacteria.
Treatment
The doctors treated the patient with the RIPE regimen. This regimen consisted of taking four drugs (isoniazid, rifampin, pyrazinamide, and ethambutol) for 2 months, followed by two drugs (isoniazid and rifampin) for 7 months. The patient was compliant with the treatment regimen and made a full recovery. The doctors assessed his ESR and CRP levels during his follow-up, and these levels had gone down. However, the necrosis of the iliac bone did not resolve.