Hereditary hemorrhagic telangiectasia, called Osler-Weber-Rendu disease, causes arteriovenous malformations in visceral organs. Hemorrhagic telangiectasia is frequently accompanied by complications, including arteriovenous malformations, which raise the danger of serious infections. However, very few occurrences of endocarditis connected to hemorrhagic telangiectasia have been documented. Although erythematous macules on the extremities are a symptom of hemorrhagic telangiectasia, they are asymptomatic. This case report is of a patient with Osler-Weber-Rendu disease, which is a rare case of infective endocarditis.
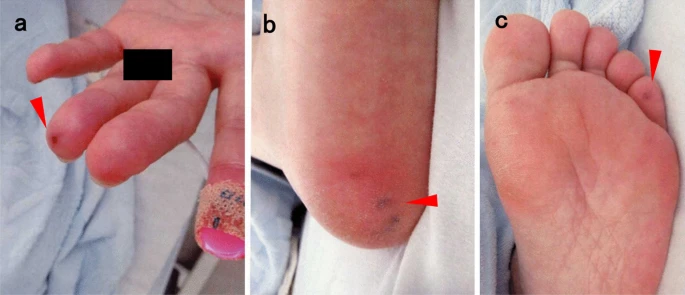
The patient was a 52-year-old Japanese woman who had been diagnosed with Osler’s illness five years prior and had a history of recurrent nasal hemorrhage. She reported having a fever and muscular pain, but she had never gotten any dental work or tooth problems in the past. She also refused that she ever used drugs. During the physical examination, pan systolic murmur and tachycardia were discovered. Moreover, skin examination revealed erythematous sensitive nodules indicative of Osler’s nodes. However, splinter haemorrhages, conjunctival haemorrhages, or Janeway lesions were not present.
With no major arrhythmia or alterations in the ST segment, electrocardiography revealed sinus tachycardia. No significant signs were suggestive of infection found during radiographic exams, including computed tomography and chest radiography. Mild mitral regurgitation was detected, and transthoracic echocardiography (TTE) revealed a left ventricular ejection fraction of 66%. Transesophageal echocardiography (TEE) was used because TTE’s subpar echo picture prevented it from determining if vegetation was present or absent. Using TEE, it was possible to see vegetation on the mitral valve’s atrial side and its anterior commissure prolapse. TEE results revealed no evidence of a perivalvular abscess.
Diagnosis and Treatment
Doctors took the blood culture, and 2 g of ceftriaxone was infused intravenously every 12 hours. However, later, Staphylococcus aureus was found, which was also methicillin-sensitive. Moreover, the presence of multiple cerebral infarctions on the MRI brain was suggestive of septic emboli. Repeat blood cultures were taken on day 3 after the start of the antibiotic treatment. However, the results were negative.
The patient had intravenous antibiotics for six weeks before being discharged with negative blood cultures. Furthermore, she was also routinely checked on in the outpatient clinic and is now making good progress with no indications of a recurrence.
Risk Factors of Hereditary Hemorrhagic Telangiectasia
One of the risk factors of HHT is an increase in cerebral infections because it causes vascular anomalies. Moreover, based on multiple studies, 47 patients (13.6%) with HHT were found to have serious infections in a retrospective examination of 353 patients. 67% of the infections among them were extracerebral, and Staphylococcus aureus was the cause for about 20% of those infections.
In several cases, extracerebral infections in HHT patients have been linked to several potential pathways. According to a theory, bacterial infiltration of the nasal mucosa because of cotton packing contributes to severe extracerebral infection worsening HHT.
Infective endocarditis linked to HHT is relatively uncommon, despite the considerable risk of acquiring serious bacterial infections.
This study is the third case report of infectious endocarditis treated successfully only with antibiotics. Skin examination is essential for the early detection of infective endocarditis. In addition, chest auscultation is also very important. The erythematous macules that HHT itself creates on the extremities typically do not have any symptoms of pain. The clinically important finding that suggested infective endocarditis in the patient of this case study was the identification of erythematous nodules with soreness (Osler’s nodes).
Conclusion
Conclusively, this is a rare case of infective endocarditis that has been encountered in a patient suffering from HHT. It is vital to recognize the risk of extracerebral infections in patients with endocarditis for early detection and to provide appropriate care.
This case study is one of the rare cases that demonstrates how important proper diagnosis of skin lesions is. Early diagnosis can prevent infective endocarditis from progressing and can help in achieving a good clinical outcome without any invasive treatment.