- Degloving injuries can present to any part of the body. However, degloving injuries of the lower limb are more common.
- Similarly, degloving injuries of the heels, upper limbs and scalp can lead to shock and severe blood loss.
- Principles of treatment of degloving injuries include preserving tissue and deluded bone through primary surgical treatment and covering it with good quality skin. Moreover, starting early mobilisation to preserve function.
A 38-year-old male patient presented to the emergency with an extensive degloving injury of the forearm. The patient tripped on the platform besides a running train. The patient was brought to the hospital intubated, ventilated and sedated.
The patient was advised a CT scan which showed a large degloving injury of the left hand up to the metacarpophalangeal joint and forearm at the level of the proximal elbow. The little finger of the patient had completely degloved starting from the proximal phalanx. Similarly, the tip of the middle finger was partially degloved in association with an undisplaced transverse fracture of the first metacarpal bone.
In addition to this, the little finger of the patient was degloving at the distal interphalangeal joint. Whereas, the ring finger was amputated at the middle of the distal phalanx. The degloved skin was amputated at the level of the underlying fascia, mechanically cleaned and rinsed with betadine and polyhexadine solution. Furthermore, the little finger and ring finger were amputated at the metacarpophalangeal joint and interphalangeal joint.
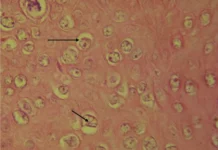
The transverse fracture of the first left metacarpal bone was reduced and plated with a mini-plate under x-ray. The degloved forearm and hand were wrapped around with the meshed full thickness graft and held in situ by skin staples. This helped cover the entire degloving defect except the hypothenar. A vacuum assisted closure of the wound was done for five days with antibiotic treatment. Full thickness skin grafts were attached after five days.

The remaining defects were covered using a free supercharged ALTP flap from the contralateral side. Similarly, an athrodesis of the PIP IV joint of the left was performed due to the posttraumatic scar contracture and posttraumatic arthrosis of the proximal interphalangeal joint of the ring finer. The degloving injuries were entirely covered.
The patient was further referred for physiotherapy because degloving injuries have a tendency to shrink in about 15% of cases, whereas, full thickness grafts in 30% of cases. In addition to this, postoperative care included applying cream to the grafted skin every day.
The patient returned to the outpatient clinic two months later with contractures at the level of the wrist of the left hand and non-compliance. The patient was advised three months of intense hand physiotherapy after which he demonstrated fist making and extension of the injured, comparable to the contralateral side.
References
Degloving Injuries of Upper Extremity: A Strategy with Full Thickness Skin Mesh https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6290308/