A case from 2018, when South African surgeons reported liver transplantation from an HIV-positive living donor and an HIV-negative recipient.
An HIV-positive mother gave birth to a child with biliary atresia who required liver transplantation. The child was 7-month-old when she was referred with end-stage liver disease secondary to biliary atresia.
Both the parents of the child were HIV-positive. Although the neonate was HIV negative at birth, the child received nevirapine daily as prophylaxis for 6 weeks.
When the mother was 27 years old, she incidentally received a diagnosis of HIV. Therefore, her doctors started her on antiretroviral therapy (ART) after 4 months of diagnosis.
She exclusively breastfed her child.
The child had previously undergone a Kasai portoenterostomy, which remained unsuccessful in establishing biliary drainage. She required liver transplantation, so her doctors put her on a waiting list in a hospital where the average wait time for liver transplantation was 49 days. However, her case was urgent, and she was on the waitlist for transplantation for 181 days with life-threatening hematemesis secondary to variceal bleeding. Her doctors shifted her to the intensive care unit, for intubation and mechanical ventilation.
She also acquired Klebsiella pneumoniae infection during the hospital stay.
The rapid decline in the child’s health warranted immediate liver transplantation. Her mother, after a constant request, was considered for liver donation. She met the criteria for being a living donor, i.e., CD4 T-cell count >200 cells/μL, viral suppression for a minimum of 6 months, no active tuberculosis infection, and no opportunistic infections.
Liver transplantation and postoperative course:
The child received a liver transplant at 13 months of age.
Preoperative immunosuppressive therapy for the mother, a night before the transplant, included raltegravir/lamivudine/abacavir. Her ART regimen remained the same.
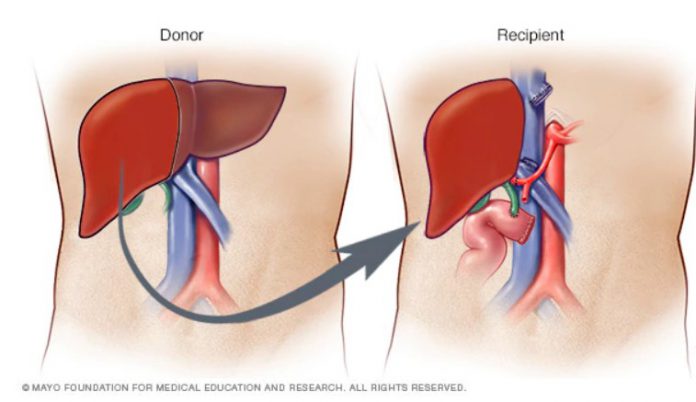
The surgeons performed a left lateral segment hepatectomy on her mother. And the child received intraoperative immunosuppression with 100 mg of methylprednisolone.
Postoperatively, the child developed pneumonia, but the infection successfully resolved with antibiotics. She also developed an epigastric collection. However, surgical drainage of the fluid along with parenteral antibiotics for Enterococcus faecium resolved the fluid and the infection. The child received standard prophylaxis for pneumocystis pneumonia and cytomegalovirus, but not for TB. Additionally, she received tacrolimus and an oral corticosteroid taper for the next 6 months.
The child was assessed for HIV, but she neither had seroconversion nor HIV-1 RNA detection.
After 225 days of transplantation, there was no evidence of HIV-1 DNA. The patient remained on tacrolimus and ART and will receive ART for at least 2 years.
References:
Botha J, Conradie F, Etheredge H, et al. Living donor liver transplant from an HIV-positive mother to her HIV-negative child: opening up new therapeutic options. AIDS 2018;32:F13–19.doi:10.1097/QAD.0000000000002000
Miro JM, Grossi PA, Durand CM. Challenges in solid organ transplantation in people living with HIV. Intensive Care Med. 2019;45(3):398-400