Tocilizumab is an interleukin-6 receptor monoclonal antibody for treating rheumatoid arthritis. It has multiple side effects; however, gastrointestinal perforation is a rare one that is fatal and requires immediate and considerable attention.
This case report is of a young male patient who has a history of RA and encountered a lower gastrointestinal perforation in association with tocilizumab therapy. Previously there was a diagnostic dilemma since the clinical presentation was the same as other autoimmune inflammatory and autoimmune diseases associated with rheumatoid arthritis. GIP is a serious infection in association with Tocilizumab especially during the COVID-19 pandemic when it is given for the management of selected patients. Furthermore, early recognition can minimize the potential risks.
Case Report
A 29-year-old Caucasian male with a h/o treatment-resistant RA came to the ER with severe generalized abdominal. The duration of the pain was three days with nausea, bilious vomiting, and watery diarrhoea. Moreover, the pain was ongoing for three weeks, however, lower in severity. He described it as colicky upper and mid abdominal pain with nausea and loose bowel movements. He denied bloody diarrhoea, mucous diarrhoea, bleeding from the rectum, melena, or hematemesis. Moreover, he didn’t have a history of symptoms of reflux either. Moreover, he denied having fever, weight loss, and rigours. In addition to that, he did not meet anyone sick or who used antibiotics recently. His systemic review was negative with no previous presentations.
Medical History
Six years prior to his presentation, his doctors diagnosed him with RA. He tried many DMARDs and biological agents. However, his clinical response was poor with continued challenging symptoms. Benepali and Baricitnib caused an episode of superficial phlebitis hence the doctors discontinued it. Moreover, adalimumab caused severe skin rash.
Doctors started him on weekly tocilizumab injections two weeks before the onset of his symptoms. He received the last dose five days before his admission. Other medications given were prednisolone and omeprazole. Methotrexate once a week and folic acid every day. His family history with respect to IBD was negative.
Index Presentation
The patient went to an OPD for evaluation a week before his index presentation. His CBC and CMP were normal. In addition, his serum antibodies for celiac were in the normal range and there was no infectious culprit in his stool panel for bacteria. Moreover, his EGD was also unremarkable. However, ileo-colonoscopy revealed very mild inflammatory changes at the distal ileum; the colon was grossly normal.
Biopsy of the terminal ileum revealed non-specific inflammation, however, there were no characteristic features for IBD. Moreover, the colonic biopsy for CMV was negative. The patient was afebrile and stable at the initial evaluation. The abdomen was generally tender without signs of peritonitis. However, the remaining examination was insignificant.
The patient’s labs showed leukocytosis and elevation in the C-reactive protein. However, the remaining tests were not remarkable. His nasopharyngeal swab for COVID19 was also negative. Moreover, the CT abdomen showed dilation in the small bowel loops in the centre of the distal ileum with fat stranding adjacently. There was no bowel obstruction or perforation and evidence of diverticular disease.
Differential Diagnosis
His differential diagnosis included IBD, infectious enteritis, and mesenteric ischemia secondary to the medium vessel and large vessel vasculitis. According to the hospital guidelines, doctors gave him broad-spectrum antibiotics for intraabdominal sepsis. Moreover, there was no elevation in his faecal calprotectin levels, in addition, bacterial and parasitical growth was also negative for stool culture.
The infectious disease team suggested getting tests done for tuberculosis enteritis due to the recent treatment via biological agents. They used QuantiFERON gold assay to test him for latent tuberculous. It was non-reactive, and his chest CT was unremarkable. PCR for Clostridium difficle, serial blood cultures for gram-negative bacteria in addition to Salmonella species were also negative.
Diagnostic Concerns
Due to the concerns of mesenteric vasculitis, a rheumatology service was consulted. Their advice was that vasculitis is rare and unusual while he was on methotrexate along with steroids. CT mesenteric angiogram was negative initially for mesenteric vasculitis. In the context of sepsis, he was given a stress dose of steroids holding methotrexate.
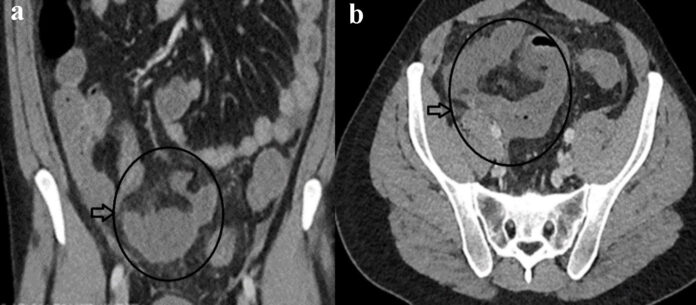
The patient’s fever spiked on day three of admission; he was also tachycardic and hypertensive. Doctors did a physical examination that revealed peritonitis in the abdomen. Moreover, his CRP level was double as well. COVID repeat nasopharyngeal test was negative and CT showed localized perforation arising from the small bowel distally with a small free fluid and air collection in the mesentery. Emergency operative intervention was recommended to control the source of sepsis.
Treatment
Doctors did a distal resection of the small bowel in addition to an end ileostomy and mucous fistula. Moreover, considering the high risk of an anastomotic leak because of local sepsis, no anastomosis was done. His post-op recovery was uneventful.
Conclusion
Histopathology of the resected bowel was negative for IBD, tuberculous enteritis and vasculitis. The likely cause of his bowel perforation was due to Tocilizumab. However, an extensive workup did not reveal any aetiology for the bowel pathology. But it was discontinued before discharge.