MRSA enterocolitis is a rare disease that usually affects patients who are immunocompromised. And although it is very common when nosocomial infections are taken into consideration, colonization in the upper respiratory tract does not lead to gastrointestinal tract migration. However, the symptoms of MRSA enterocolitis comprise the pseudo membrane, which is seen on colonoscopy. For example, abdominal pain and diarrhoea, the illness is misdiagnosed very commonly as Clostridium difficle infection or a virus. Moreover, although some cases of MRSA enterocolitis have been reported and published in adults or infants, this case study is the first ever in a toddler with MRSA enterocolitis.
This case is about an unexplained increase in frequent diarrhoea or ostomy output, which emphasizes leading to stool culture screening for MRSA. In addition, other common pathogens of the GI are as well.
Case Study: MRSA Enterocolitis
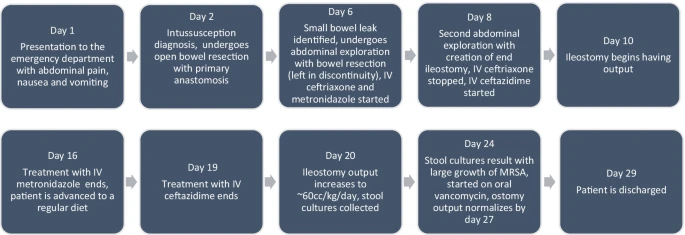
An apparently healthy 16-month-old non-Hispanic White toddler presented to the emergency hospital with 2 days of abdominal pain and emesis. He had no prior medical or mental history. Only the patient’s father suffered constipation, which was found after the family history. The patient did not face any monetary, linguistic, or cultural barriers while living. Moreover, he lived at home with his parents and sister. Doctors did a physical examination at admission was within normal ranges, and in particular, his abdomen was soft, non-distended, non-tender to palpation, and free of any masses. His intussusception was identified, and it was successfully treated by radiology using a water-soluble contrast enema.
He was brought for a repeat contrast enema to be evaluated for recurrence intussusception the next day because his symptoms had persisted. The contrast enema did not reveal any signs of recurrence. In addition, a computed tomography (CT) scan was also performed to provide more information. Although a CT scan did not reveal intussusception, it did highlight a potential small intestinal obstruction due to a weakened intestine.
Physical Examination
His physical examination was still within normal ranges. However, he seemed uneasy since he was suffering from increased fussiness and was also agitated. Moreover, the patient’s history raised concerns about recurring intussusception that might necessitate surgical reduction. After the surgical examination, the doctors discovered that the patient had intussusception in his terminal ileum. This was manually decreased, but it was discovered to contain little intestinal necrosis. Furthermore, it was removed with a primary, end-to-end anastomosis, and an appendectomy was carried out. The postoperative pathology report identified the material as being from the small intestine and described it as having ischemia necrosis, intraluminal fibrin, and pieces of necrotic bowel mucosa.
Further Emergency Intervention
An anastomotic leak and three small intestine perforations on hospital day six exacerbated the toddler’s condition. Because of this, he required an exploratory laparotomy with abdominal washout, and small bowel resections, in addition to a temporary abdominal closure. His pathology revealed patches of patchy ischemia necrosis, serositis, and many transmural abnormalities in the small intestine. However, he was brought back two days later for the construction of a mucous fistula to close the ileostomy. The doctors removed 20–30 cm of the small bowel in total.
Post-Op Treatment
The toddler was treated with IV ceftriaxone and metronidazole as part of his surgical care, followed by ceftazidime and metronidazole. On hospital day 10, he resumed having bowel movements after being started on total parenteral nutrition (TPN) on hospital day 9. Furthermore, on the 19th day of the hospital stay, the TPN and antibiotics were removed, and he was moved to a regular diet. He experienced two episodes of nonbilious emesis on hospital day 20, and his ileostomy output was high at 50–60 mL per kg per day. The patient’s abdominal exam was still being conducted normally at this point.
He had a pink, patent, and functional ostomy. The doctors also prescribed him replacement fluids. Other than that, stool cultures were also taken. However, although he went through therapies like loperamide, with a change in meals, and treatment of electrolyte imbalances, his ileostomy output remained high. He was otherwise symptom-free, tolerating a diet, and had normal test results and a physical examination during this time. On day 24 of the hospital stay, stool cultures were performed. All save a significant growth of MRSA were negative. Following a diagnosis of MRSA enterocolitis, the patient began receiving 13 mg/kg of oral vancomycin three times per day. The toddler tolerated it well, and by day 27 of hospitalisation, his ostomy output had returned to normal. On the 29th hospital day, the patient was released to go home in good condition.