The image above shows a transilluminating newborn’s head, affected by Herpes Simplex virus (HSV), leading to encephalitis and causing extensive damage to the cerebral tissue which then gets replaced by the saclike accumulation of fluid, thus the transillumination. Neonatal bedside transillumination a diagnostic test, rather a screening tool
Neonatal herpes simplex virus infection
It has high morbidity and mortality with an incidence of one in 3,000 to one in 20,000 live births. Incidence is higher when the mother has an active primary genital HSV infection at the time of delivery or late in the third trimester. Reactivation of HSV in mothers is associated with lower transmission risk. Most of the cases of neonatal HSV infection are transmitted during birth, while transplacental and hospital-acquired being responsible for a handful. HSV type 2 being a more common culprit than type 1. It is noteworthy that only 30% of the affected neonates have mothers with symptomatic HSV.
Signs And Symptoms
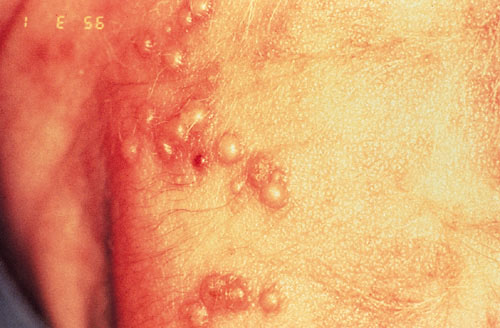
Affected neonates may show signs and symptoms between 1 to 3 weeks of life and less commonly up to the 4th week, varying from skin vesicles to localised CNS disease to widespread infection (causing hepatitis, adrenalitis, encephalitis, DIC, etc.).
If former is the case, then a more serious form of the disease may take its course over a period of 7 to 10 days, if left untreated.
4% of the neonatal HSV infections are congenital HSV infection, in that case, the infant may present with microcephaly, vesicular skin lesions, hydrocephalus and chorioretinitis.
The case in discussion here is of HSV causing localised CNS infection: encephalitis.
This can present with fever, neurologic findings such as convulsions, hypotonia, apnea, lethargy, etc, CSF pleocytosis, and increased protein concentration. Skin, eyes, and mouth may or may not be involved
Unfortunately, the infection of this newborn remained undiagnosed during his hospital stay, due to which 90% of his brain tissue was damaged.

Diagnosis
Although a rapid diagnosis is a key to successful treatment, it is initially difficult to promptly diagnose due to vague and non-specific symptoms like lethargy, irritability, hypotonia, etc.
Viral culture or HSV PCR is essential, for which fluid from skin vesicles is tested. In neonates especially, skin findings are usually absent and the virus inhabits the CNS only.
Therefore, infants require a high index of suspicion. Suspect HSV infection in all neonates presenting with nonspecific symptoms such as fever, poor feeding, hypotonia or seizure within the first month of life. Culture any vesicular rash if present till eight weeks of life and immediately start parenteral antiviral, not awaiting the culture results. CSF PCR should be performed.
However, if HSV encephalitis remains undiagnosed, it has devastating effects that cannot be reversed even with antiviral therapy.
Treatment
Parenteral antiviral therapy is the treatment of choice for all suspected and diagnosed neonatal HSV infections, for 14 days if the disease is localised and 21 days if disseminated or if the central nervous system is involved.
How to prevent neonatal transmission?
- Obtain history of HSV infection during the first prenatal visit.
- Prophylactic acyclovir if active lesion at the time of labour, in the third trimester or in cases of frequent outbreaks.
- In mothers with active genital lesions, avoid vaginal delivery and fetal scalp monitoring.
References
– CAROLINE M. RUDNICK, M.D., PhD, St. Anthony’s Medical Center, St. Louis, Missouri GRANT S. HOEKZEMA, M.D., St. John’s Mercy Medical Center, St. Louis, Missouri Am Fam Physician. 2002 Mar 15;65(6):1138-1142.
https://www.aafp.org/afp/2002/0315/p1138.html
– https://www.msdmanuals.com/professional/pediatrics/infections-in-neonates/neonatal-herpes-simplex-virus-hsv-infection




