This case is of an 87-year-old woman with recurrent fever and severe perineal pain for two weeks. However, she denied recent changes in her bowel movement, abdominal pain, blood in her stool, diarrhoea, vomiting, melena, or urinary symptoms. Moreover, she had no shortness of breath or cough. The systemic review did not contribute to her presentation.
Medical History
Her past medical history was significant for uncontrolled diabetes mellitus type II, Crohn’s disease diagnosed 18 years ago, hemicolectomy for perforated ileocecal disease, and chronic secretory diarrhoea due to malabsorption of bile acids. In addition, she also had GERD and hypertension.
The patient underwent a surveillance colonoscopy recently, three weeks prior to her presentation. اربح المال من الالعاب However, it was unremarkable other than the hyperplastic polyp in the lower rectum removed through a cold snare. Moreover, her random ileocolic and colonic anastomosis biopsies were negative.
Doctors did a physical examination; she appeared ill and febrile with a pulse rate of 110 beats per minute and low blood pressure of 95/65 mm Hg. The abdomen was non-tender and soft to examine. Moreover, the perineal examination was remarkable for a necrotic-looking, black in colour eschar on the left ischioanal region with profound changes in cellulitis. There was no palpable bullae or crepitus, and the systemic examination was unremarkable.
Diagnosis – Gemella morbillorum
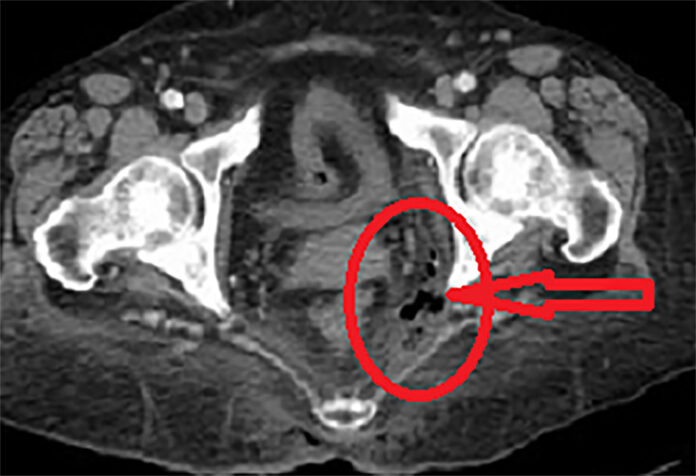
Doctors also did a CT scan of the pelvis revealing soft tissue gas within the left ischiorectal fossa. Moreover, there was no evidence of fluid collection or abscess formation. There were no signs of fistulous communication and rectal perforation either, in addition to no features of Chron’s colitis. لعبه البوكر لعبه البوكر
Doctors gave her broad-spectrum antibiotics based on the guidelines for necrotizing soft tissue infections generated from local susceptibility patterns. Moreover, he went through an emergent debridement of perineal necrotic tissues at the base of viable tissues. However, no communication between the deep wound cavity and the rectal wall was seen.
Her doctors obtained two blood cultures at admission, which grew Gram-positive cocci in chains. بينجو لعبة Moreover, the subsequent cultures only grew Gemella morbillorum. Echocardiography ruled out concurrent infective endocarditis and transesophageal echocardiogram showed negative results for valvular vegetations.
Treatment and Follow Up
Doctors did daily wound dressing and VAC dressing in situ. It enhanced wound healing. She was transitioned to oral clindamycin and amoxicillin according to susceptibility results. However, at least two weeks of antimicrobial therapy was prescribed as per consultation.
A four week follow up revealed good healing of the wound.