A patient presented to the emergency department with complaints of sudden onset of visual disturbance, slurring of speech, dizziness, and left-sided facial drop. The patient had no complaints of any bulbar symptoms, sensory disturbances, headache, or sphincter disturbances. History revealed that the patient was a known case of non-insulin-dependent diabetes mellitus.
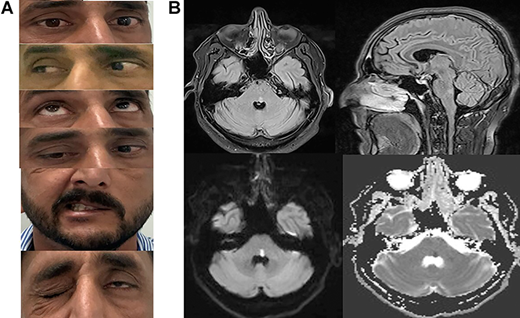
Physical examination revealed left horizontal conjugate gaze paresis, and upon looking left, the patient’s left eye showed limited adduction with associated nystagmus of the right eye. The convergence was spared indicating left internuclear ophthalmoplegia. Vertical movements of the eyes were normal. On further examination, flattening of the nasolabial folds were appreciated with the inability to fully close the left eye and deviation of the right side. The rest of the neurological exam was normal.
A non-contrast magnetic resonance imaging of the brain was performed which showed tegmentum hyperintensity of the left lower pons on FLAIR (fluid-attenuated inversion recovery) images, and hyperintensity on diffusion-weighted images (DW) and hypointensity on apparent diffusion coefficient (ADC) suggesting a left pontine acute ischemic stroke.
CT angiogram of brain and neck vessels revealed no abnormalities. Other routine laboratory investigations, thrombophilia work-up, and ECHO were normal.
The patient was diagnosed with Eight-and-a-half syndrome.
The patient was started on dual antiplatelet drugs and a lipid-lowering drug, atorvastatin. His blood pressure was controlled and optimized. Facial exercises were advised to improve the left-sided drooping of the face. His eyes were patched alternately, which improved the blurry vision.
Eight-and-a-half Syndrome
Eight-and-a-half syndrome is a rare neuro-ophthalmic syndrome which gets its name from the following combination:
- Ipsilateral conjugate horizontal gaze palsy (the “one”)
- An ipsilateral internuclear ophthalmoplegia (INO) (the “half”)
- Seventh nerve palsy.
One-and-a-half syndrome with the 7th nerve palsy together is called the eight-and-a-half syndrome. This syndrome is usually due to lesions at the level of the pons, most commonly due to ischemic stroke. Other causes of pontine lesions may include demyelinating lesions such as multiple sclerosis and space-occupying lesions such as tuberculoma.
Vascular etiology is the most common there patients with the eight-and-a-half syndrome usually present with abrupt onset of symptoms. No age, race, or sexual predilection has been seen. However, the risk factors are the same as for vascular pathologies, i.e. diabetes mellitus, hypertension, hyperlipidemia, and hypercholesterolemia.
The abrupt onset of symptoms as in our case suggested ischemic stroke. Prognosis depends on the size of the infarct and the ability of the affected area to recover. Usually, facial palsy improves first followed by the ocular symptoms. The treatment depends on the underlying etiology, in addition to neurorehabilitation
Prompt and urgent localization of the lesion with imaging studies is imperative as the prognosis is dependent upon the size of the infarct and the ability of the affected area to recover.
Management depends upon the etiology, but neuro-rehabilitation is usually indispensable.
References:
Nandhagopal R, Krishnamoorthy SG. Neurological picture. Eight-and-a-half syndrome. J Neurol Neurosurg Psychiatry. 2006;77(4):463. DOI:10.1136/jnnp.2005.078915
Mesina BVQ, Sosuan GMN, Reyes KB. Eight-and-a-half syndrome: a rare, potentially life-threatening disease. GMS Ophthalmol Cases. 2018;8:Doc04. Published 2018 Mar 8. DOI:10.3205/oc000086
Hassan A Ahmed, Omar Y Al Assaf, Hamdan M Alzarooni, Pournamy Sarathchandran, Clinical findings of eight-and-a-half syndrome, Oxford Medical Case Reports, Volume 2020, Issue 10, October 2020, omaa087, https://doi.org/10.1093/omcr/omaa087