A patient referred to and from the emergency department until a final diagnosis
was made— An unremarkable initial visit to the ED rapidly worsened within a few
hours ultimately taking the patient to the operation theatre and ICU.
A 16-year-old female patient was brought to the emergency department with complaints of abdominal pain, nausea, headache, generalised body pain, and breathlessness for the past 3 days. She pointed to her right upper quadrant when inquired about abdominal pain. The pain neither radiated nor had shifted and was achy in character. The patient was a known case of asthma. لعبة الحظ الحقيقية Upon further inquiring about the other organ systems, the patient revealed that she had recently noticed a lump in her right breast. Her last menstrual period was 3 weeks back, during which she used tampons. طريقة الربح في الروليت She was an avid swimmer. The patient was not sexually active. لعبة بينغو
General Examination:
The patient appeared well and was not in distress. All her
vital signs were normal, except for a slightly increased heart rate.
Abdominal Examination:
Abdominal examination revealed mild right upper quadrant
tenderness. Peritoneal signs were absent.
Breast Examination:
Palpation of the right breast revealed slight tenderness inferior to the right areola. No fluctuance, erythema, or obvious lump was appreciated.
The rest of the examination was unremarkable.
Chest radiography, abdominal ultrasound, and laboratory evaluation were normal. The patient’s tachycardia improved with intravenous hydration and her myalgias improved with intravenous ketorolac.
The patient was discharged with advice to return to the emergency
department if her condition worsens and follow-up with her OB/GYN.
Referral to OB/GYN:
The patient was then brought to her OB/Gyn with complaints
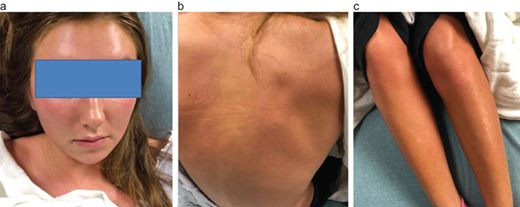
of worsening of her breast lump and a diffuse rash. On examination, the patient
appeared flushed and ill, and she was pyrexic with a temperature of 101.4°F. The
patient was having chills, and full-body erythema was noticed. Inspection of
the right breast didn’t reveal any swelling, erythema, lesions, or scars. On
palpation, there was a deep 2.5-cm exquisitely tender nodule located inferior
and lateral at the areolar border of the right breast.
Second Visit to the Emergency Department:
The patient was given acetaminophen and was referred back to the emergency department after the OB/Gyn excluded gynecological causes of her condition.
General Examination:
On her second visit to the ED, her vitals revealed body
temperature of 98.6°F, heart rate of 102 beats/min, blood pressure of 92/47
mmHg, and respiratory rate of 17 breaths/min. Saturation of oxygen on pulse
oximetry showed a reading of 99% on room air.
Examination in the ED revealed diffuse blanchable diffuse
full-body macular erythroderma.
Abdominal Examination:
Same as during the first visit.
Breast Examination:
Breast examination revealed the known deep 2.5-cm extremely
tender nodule just like reported by her OB/GYN, but this time the breast
examination also revealed overlying erythema consistent with cellulitis.
Investigations:
Repeat laboratory investigations revealed:
▪ White blood cell count of 17 (4.5–13 bil/L)
▪ Alkaline phosphatase of 136 (37–134 U/L)
▪ Aspartate aminotransferase of 122 (10–37 U/L)
▪ Alanine aminotransferase of 151 (5–20 U/L)
▪ Total bilirubin of 1.4 (0.3–1.2 mg/dL)
▪ Lactic acid of 1.3 (0.5–2.2 mmol/L)
▪ Creatinine kinase of 50 (30–150 U/L)
▪ Influenza A/B, respiratory syncytial virus, and infectious mononucleosis by nucleic acid amplification were negative
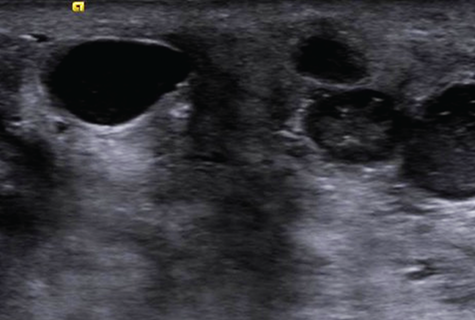
During the second visit to the ED, an ultrasound of the
right breast was performed, which showed several cystic areas, the largest one measuring
up to 2.0 × 1.0 × 1.3 cm. These areas demonstrated internal debris and
posterior acoustic enhancement.
A working diagnosis of toxic shock syndrome (TSS) secondary
to a breast abscess.
A pelvic examination of the patient was required but denied.
The patient was started on intravenous vancomycin, but her condition continued
to decline despite appropriate therapy with fluids, antibiotics, and
norepinephrine. She was shifted to the intensive care unit where a pelvic exam
was performed, revealing no acute process or foreign body.
The patient was taken to the operation theatre for incision
and drainage of her right breast abscess. Multiple purulent abscesses were
noted. Debridement was performed, and samples were sent for culture and sensitivity
which grew Staphylococcal aureus methicillin-resistant before Staphyoccal
aureus (MRSA), susceptible to both vancomycin and clindamycin.
The patient substantially improved and was
discharged on day 4 on oral clindamycin to be continued 10 days. At the 1 month
follow-up, the patient had recovered completely and returned to her competitive
swimming.