A 52-year-old Chinese male presented to the outpatient department with complaints of bloating, constipation, and abdominal discomfort for the past 1 week. Three days before presenting, he developed a mild cough, and on the day of admission, he developed dyspnea and palpitations.
Past Medical History:
His past medical history was positive for diabetes mellitus, hypertension, and dyslipidemia. The patient had a myocardial perfusion scan for exertional dyspnea 2 years back, which was negative for ischemia with an LVEF of 55%.
Family History:
There was no family history of cardiovascular diseases.
Social History:
The patient consumed approximately 4 bottles of beer per day for the past 30 years. He was an avid smoker, using an e-cigarette. Usually, he used one cartridge for three days in his e-cigarette, but for the last 3 months, his smoking had escalated to one cartridge per day.
Examination:
The patient was admitted for evaluation. On examination, his vitals were:
- Blood pressure of 128/93 mmHg,
- Heart rate of 214 bpm,
- Temperature of 36.7 °C
- Oxygen saturation of 98% on room air.
On chest examination, lungs were clear on auscultation, and no murmurs were heard. Abdominal examination revealed a soft, non-tender, but distended abdomen. Bowel sounds were normal and there was no lower limb edema.
Serological investigations:
Blood samples were withdrawn for serological investigation which gave the following results:
- Serial Troponin-T of 32, 35 and 28 ng/L (normal range < 30 ng/L).
- NT-proBNP (2,594 pg/ml) (elevated).
- White blood cell count of 12.8 × 103/uL.
- Serum creatinine was elevated to 174 umol/L as compared to 109 umol/L just three months prior.
- Serum lactate was 6.7 mmol/L (abnormally high).
- Hemoglobin, inflammatory markers, electrolytes, thyroid, liver function tests, C-reactive protein, and procalcitonin were normal
- Arterial blood gases gave the following results:
- pH 7.050
- pO2 138 mmHg
- pCO2 41 mmHg
- bicarbonate 11 mmol/L
The above ABG values indicated metabolic acidosis with respiratory compensation.
Cardiomegaly and pulmonary congestion were observed on the chest radiograph. ECG revealed atrial fibrillation (AF) with a rapid ventricular rate of 218 bpm.
Intravenous amiodarone infusion was started. Respiratory distress worsened due to acute pulmonary edema warranting intubation. The patient was started on intravenous diuretics.
Other imaging studies:
An urgent TTE during AF showed:
- Non-dilated left ventricle
- LVEF of 10-15% with global hypokinesia
- Mildly dilated right atrium
- Mild mitral regurgitation
- Moderate to severe tricuspid regurgitation
- Estimated right ventricular systolic pressure (RVSP) of 38 mmHg
No intracardiac thrombus was seen on the transesophageal echocardiogram.
Color doppler revealed an incidental small inferior sinus venosus ASD of 0.6 cm with predominantly left to right shunting.
Amiodarone was stopped due to severe derangement of the liver function tests. The patient’s heart rate remained between 130-160 bpm despite maximally tolerated doses of digoxin and bisoprolol.
Synchronized direct current cardioversion (DCCV) was performed but resulted only in transient conversion to sinus rhythm. Eventually, after one week, the heart rate slowed down, and spontaneously converted to sinus rhythm on the 8th day of admission.
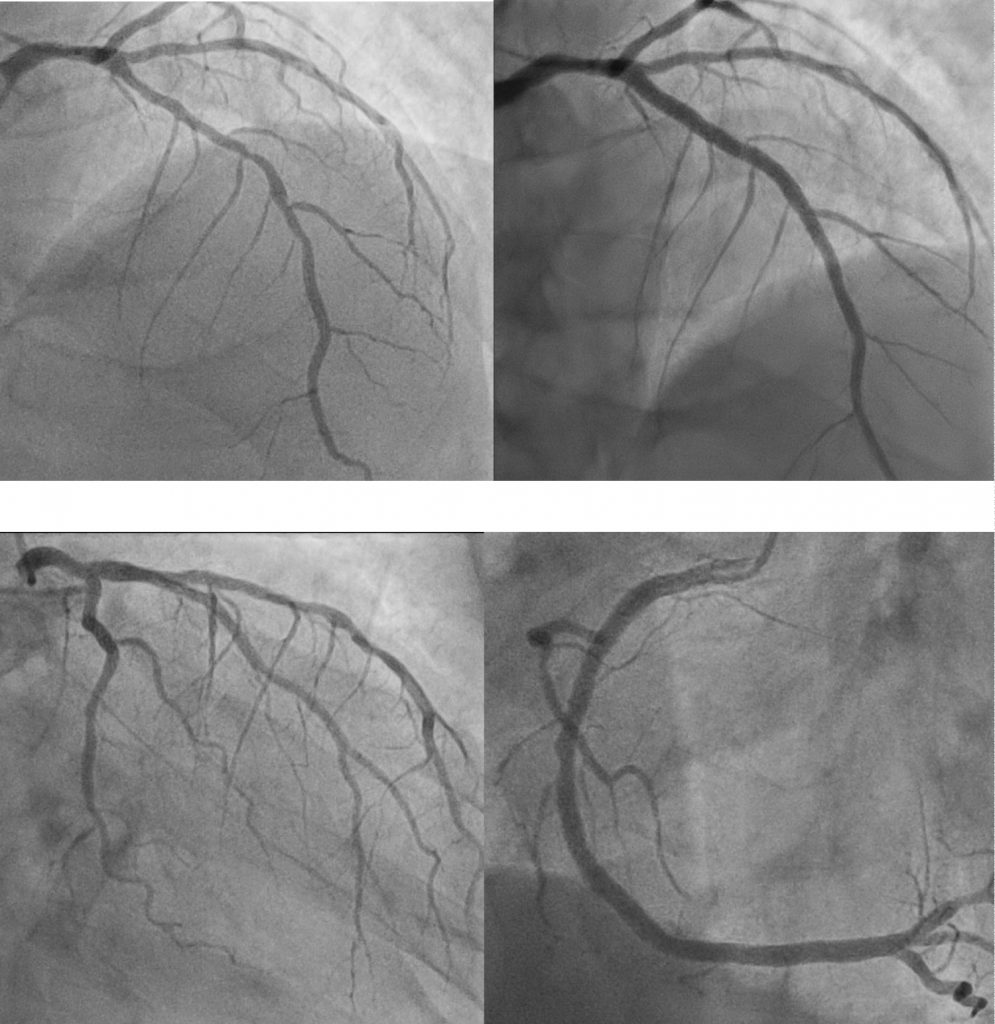
Coronary angiography showed diffuse 50-65% stenosis in the LAD artery, luminal irregularities in the left circumflex artery, and 30% stenosis in the mid-right coronary artery. Fractional flow reserve (FFR) measurement in the LAD was 0.72 and improved to only 0.80 after deploying two overlapping drug-eluting stents (DES) in the ostial to mid LAD.
The patient was diagnosed with congestive cardiac failure secondary to predominantly non-ischemic cardiomyopathy with underlying single-vessel coronary artery disease following a short period of increased e-cigarette usage.
The patient was counseled regarding smoking cessation and fluid restriction. He was given triple anti-thrombotic therapy post-PCI and high-intensity statin post-PCI, along with angiotensin-converting enzyme inhibitor, beta-blocker, and aldosterone antagonist.
Source: LIM B, LEE S, CHAI SC (2020) Vaping Induced Cardiac Complications – A Smokescreen Coming to Engulf the Heart?. Int J Clin Cardiol 7:202. doi.org/10.23937/2378-2951/1410202




