An 8-year-old girl from Bangladesh developed disseminated histoplasmosis!
She presented with complaints of fever and jaundice. She had abdominal distension for two and half months. However, she did not have any history of contact with a TB patient or travel to an endemic malarial zone. She was also negative for any previous history of jaundice or any blood disorders.
On general physical examination, the girl looked severely wasted and stunted. She was pale and her eyes clearly indicated jaundice. The doctors however found her vitally stable. Her skin showed signs of infected scabies and the doctors also noticed that she lacked BCG scar marks. She had ascites and generalized lymphadenopathy. Moreover, her liver and spleen were enlarged too.
A spectrum of Investigations Reveal Histoplasmosis
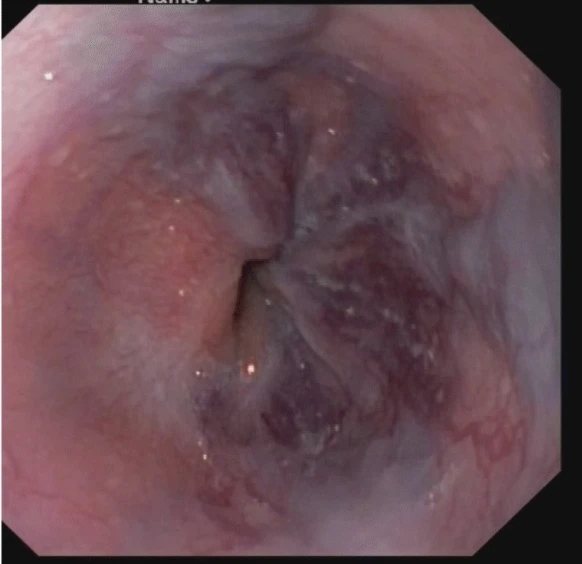
After a thorough physical examination, doctors subjected the girl to a ton of investigations. Her blood profile indicated mild anaemia, neutrophilic leukocytosis and thrombocytosis. Her ESR was elevated, indicative of an inflammatory process. The LFTs displayed hyperbilirubinemia and mildly decreased albumin. However, her ALT levels were normal. Doctors also did an ultrasound of her abdomen. It revealed splenomegaly and a mildly dilated biliary system. Furthermore, endoscopy indicated grade four oesophagal varices. The histology of a lymph node resected from the patient dropped conclusive findings. It showed the presence of giant cells and a granuloma. Doctors found numerous PAS-positive Histoplasma capsulate
Disseminated Histoplasmosis: An Insight
Histoplasmosis refers to a fungal infection caused by Histoplasma capsulati. Most of the time, the infection does not result in any symptoms and resolves on its own. Only sometimes does it require treatment and only rarely does it develop into a disseminated form. When present, it usually starts off in the alveoli and pulmonary disturbances are its primary manifestations. However, it then spreads to the reticulo-endothelial system and affects the spleen and liver causing hepatosplenomegaly. Common symptoms that the patients present with include fever, weight loss and respiratory problems. The clinical features depend mainly on the immune status of the patient and usually it is the immunocompromised who have to bear the brunt of the disease. Still, the disseminated form of the disease is rare and because our patient had the disease spread to her biliary tract, she had obstructive jaundice and ascites.
Histoplasmosis and TB
In areas where TB is endemic, patients of histoplasmosis are often mistaken for tuberculosis. Because both of these have many similar clinical manifestations, at times it becomes very difficult to differentiate between the two, especially in patients who have AIDS too. Various tests that are then employed to make a definitive diagnosis include culture examination, fungal stains, blood smears and lymph node biopsies. Moreover, doctors also use Histoplasma antigen test in urine for rapid diagnosis.
Apart from affecting the respiratory and hepato-biliary system, histoplasmosis can also involve the gastrointestinal tract and adrenal glands. Of particular interest is the fact that sometimes it can also manifest as hypercalcemia because of the active vitamin D form secreted by the granuloma that is formed in histoplasmosis. Furthermore, it has all the potential to trigger pancytopenia by affecting the bone marrow. Hence, doctors need to keep these atypical involvements in mind while looking at a patient with a combination of these features.
Treatment of the Patient
Doctors initiated the patient’s treatment with deoxycholate Amphotericin B. They also gave her Permethrin for her scabies. To treat her varices, they did an endoscopic variceal ligation. Fortunately, she did not develop any complications during the course of her treatment and her symptoms resolved pretty well. Her fever subsided, jaundice resolved and her organs dropped down to their typical sizes too.
On showing improvements, the doctors discharged the patient along with a prescription of Itraconazole and propanolol. They advised her to take them for a few months. Doctors called her for a follow-up after due time. She had regained weight and was afebrile. On endoscopy, she did not have any varices. Doctors also did a follow-up ultrasound to look for any changes in organomegaly. They noticed that her biliary system was normal and there was no splenic enlargement. However, her liver still showed slight hepatomegaly. Overall the treatment was successful with significant improvements in the patient’s condition.