Anorectal mucosal melanoma, a rare and aggressive neoplasm
Anorectal mucosal melanoma is a rare and aggressive type of neoplasm. However, because melanoma has rare and nonspecific symptoms, it is often diagnosed late and, therefore, has a 10% 5-year survival rate. For this reason, surgical resection remains the standard treatment for anorectal melanoma. In a similar case, an 81-year-old woman presented with a 6-month history of perianal pain, complete constipation, tenesmus, anal secretion, and hematochezia. Whereas the patient denied any weight loss, inguinal mass, pruritus, or diarrhoea.
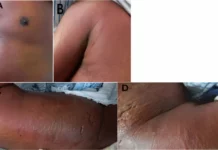
She visited a general practitioner earlier because of the presence of blood in the stool and an anal nodule. The doctor diagnosed her with thrombosed haemorrhoids. Her past medical history was also significant for hypertension and diabetes mellitus type 2. Physical examination showed a prolapsed melanocytic nodule in the anal canal, measuring 5 cm. The nodule was hard on palpation. Digital examination showed no evidence of sphincter involvement or inguinal lymphadenopathy. Doctors further advised a biopsy which confirmed the diagnosis of anorectal melanoma.
Investigations and prognosis
Doctors further advised a complete colonoscopy to rule out a synchronous lesion. Computed tomography of the chest, abdomen, and pelvis was significant for metastatic disease, with hepatic, lymphatic, and adrenal involvement. Doctors also suspected n anal tumour resection because the patient continued to have difficulty in defecation with bleeding and severe pain. Doctors resected the tumour with partial resection of the anal sphincter. She was discharged a day after the procedure.
The patient showed significant improvement in symptoms in the outpatient follow-up. Pathological examination of the tumour was consistent with the diagnosis of anorectal mucosal melanoma. After consulting the clinical oncology team, doctors decided to not proceed with chemotherapy considering the patient’s advanced age, comorbidities and poor response rate of treatment. After 5 months of the surgical procedure, the patient’s anal lesion relapsed and she developed anal bleeding. Doctors advised one session of hemostatic radiation therapy for palliation.
The patient died 10 months after the surgical procedure because of multiple liver metastases and liver failure.
Source: American Journal of Case Reports