An 86-year-old female, previously treated for bilateral breast cancer, presented to the hospital. Only this time, she reported feeling a mass in her gastric region.
Doctors diagnosed her with invasive ductal carcinoma of the right breast when she was 72. She underwent total mastectomy with level 2 axillary lymph nodes resection. 7 years later, breast cancer reemerged in her left breast. Doctors again performed a total mastectomy so that she lost both her breasts along with level 2 lymph nodes resection, this time in her left axilla. Interestingly, both of her cancers turned out to be ER and PR positive, on immunohistochemistry. Breast cancers that express these receptors have a good prognosis.
Breast Cancer Knocks the Door a Third Time Around!
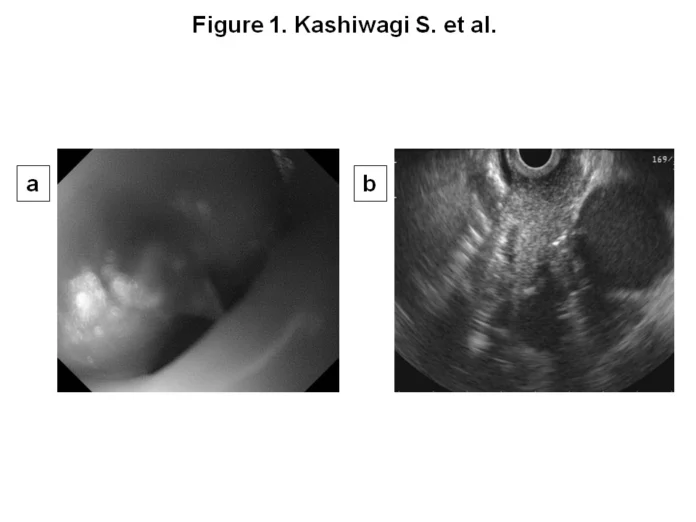
On her current presentation, the patient also reported having profound dysphagia. Doctors did an esophagoscopy which revealed a submucosal lesion in the middle third of her oesophagus. Moreover, they also diagnosed a tumour in the cardiac region of her stomach. Both of these findings later accompanied an elevated level of squamous cell carcinoma antigen in the serum.
The next step was to do a biopsy to disclose the actual nature of the lesions. However, just before that, doctors subjected the patient to a mediastinal CT to determine the extent of the oesophagal lesion. It revealed its spread to tracheal bifurcation so as to involve the left primary bronchus too. Anyhow, after taking biopsy specimens from the oesophagus and stomach, the doctors sent them for histopathology. Results rolled back and confirmed that oesophagal lesion was a poorly differentiated adenocarcinoma quite shockingly positive for ER (estrogen receptor). Yes, breast cancer had re-emerged in the oesophagus now. However, for gastric tumours, the doctors did not notice any ER or HER2 positivity and labelled it a primary gastric adenocarcinoma with moderate differentiation.
Breast Cancer Metastasis
Breast cancer only rarely metastasizes to GIT let alone to the oesophagus. The literature describes only 20 such cases where breast cancer presented as a metastatic lesion in the oesophagus, that too in the submucosa thus leading to severe dysphagia. This type of metastasis causes dysphagia due to either causing stenosis of the oesophagal lumen or by compressing the oesophagus. Compression results when the malignancy spreads outside the wall thereby putting pressure on the oesophagus and closing the lumen. In all such cases, however, the mucosa remains unaffected. Hence, mucosal biopsies do not breed a diagnosis. Doctors usually take biopsy specimens from submucosa under ultrasonic guidance and make their diagnosis based on histological reports and staining characteristics. Breast cancers usually turn out positive for hormone receptors such and ER and PR.
Prognosis
The prognosis for rare occurrences is never straightforward. In fact, because of the lack of adequate databases and literature reviews, doctors usually consider the prognosis for metastatic breast cancer in the oesophagus, poor by default. Therapeutic strategies are designed keeping in mind the characteristics of the lesion and include surgery, radiation and chemotherapy. With surgery, the risk of post-operative death comes out very high because oesophagal metastasis requires highly invasive surgery. Other cases involve stenting to relieve dysphagia followed by either radiation therapy or therapy with cytotoxic drugs and hormone antagonists. Carcinomas that express hormone receptors (ER, PR and HER2) show a good prognosis. In such cases, hormone therapy shows impressive results. Nevertheless, doctors should employ multiple therapy solutions after carefully analyzing cancer for its histological subtype.
Treatment of Our Patient with Breast Cancer
Because of the advanced age and general ill health of the patient, doctors did not consider surgery despite progressing dysphagia. Moreover, they focused more on oesophagal cancer than on gastric one. They initially employed radiation therapy to reduce the size of the lesion. It worked and made intubation possible. Next, they started the patient on chemotherapy with drugs such as cyclophosphamide. They also gave her hormone therapy (medroxyprogesterone) owing to the fact that her cancer expressed hormone receptors. Her gastric cancer however did not improve much. Doctors did not operate on it because of a significant risk of bleeding. Her gastric lesion had invaded the submucosal layer.
Metastatic cancer showed a good treatment response. They also kept the patient on chemo-hormone therapy in the OPD for quite some time. No progression in the disease has been noticed since.