Moxifloxacin-Induced Black Hairy Tongue
Black hairy tongue (BHT) is a rare benign condition with a reported prevalence ranging from 0.6% to 11.3% depending on age, gender, ethnicity, and study population. BHT can be caused by both intrinsic and extrinsic factors, and while several antibiotics have been linked to BHT, no previous reports of moxifloxacin-induced BHT have been published. This is, as stated in the study, the first report of moxifloxacin-induced BHT.
This article describes the case of a woman who presented with a brown and hairy tongue with a history of mixed connective tissue disease. She was taking prednisolone for mixed connective tissue disease when she developed right finger flexor tenosynovitis, which was complicated by Mycobacterium chelonae osteomyelitis. Based on the susceptibility results, she was treated for 6 weeks with tobramycin, imipenem, and clarithromycin before switching to moxifloxacin and clarithromycin. She developed brown discoloration on the dorsum of the tongue within 10 days, along with carpet-like elongated filiform lingual papillae. The BHT diagnosis was made. Improvement was seen within 2 days of discontinuing moxifloxacin, and her right finger has shown no signs of recurrence for 12 months.
Case report
A 69-year-old woman presented to our clinic with brown discolouration of the tongue and a history of mixed connective tissue disease (MCTD), hypertension, hyperlipidemia, diabetes mellitus, and osteoporosis. For the MCTD, she was taking oral prednisolone 5 mg once daily. She had debridement and reconstruction surgery about 3 months before her presentation for magnetic resonance imaging-proven right index and middle finger flexor tenosynovitis, which was complicated by osteomyelitis caused by Mycobacterium chelonae. Based on the susceptibility results, an induction therapy regimen of intravenous tobramycin, imipenem, and oral clarithromycin was initiated. Similarly, she was given antibiotics for a total of six weeks before being switched to oral moxifloxacin and clarithromycin.
She noticed changes in her tongue colour within 10 days of the switch and presented to the clinic without fever, nausea, or taste changes. However, she denied using any different medications, taking any herbal/traditional Chinese medicine, smoking, or drinking. She also denied using irritant/oxidizing mouthwashes, tongue cleaners, or tongue scrapers.
Investigations and findings
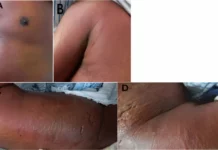
She was found to be in good general health upon examination, with a blood pressure of 135/76 mmHg, a pulse of 80 beats per minute, and a respiration rate of 15 breaths per minute was recorded. Whereas a body temperature of 36.7°C. The oral mucosa was dry, and there was little saliva on the tongue’s floor. The brown discolouration was visible on the tongue’s dorsum, with carpet-like elongated filiform lingual papillae. There were no signs of tooth decay, halitosis, discharge, bleeding, or exudates. Her gingiva was free of trauma and clear. She didn’t wear dentures. Her right finger was healed, and the rest of her clinical exams were also unremarkable.
There was no tongue swab culture. The preliminary diagnosis was stained tongue caused by foods or BHT caused by antibiotics. Based on the rapid onset of her tongue discolouration, other differential diagnoses such as oral hairy leukoplakia and acanthosis nigricans were ruled out. Her tongue discolouration and elongated filiform lingual papillae did not improve after two weeks of daily oral hygiene and tongue scraping. As a result of her wishes and the lower susceptibility of moxifloxacin to isolated Mycobacterium chelonae than clarithromycin, we discontinued moxifloxacin and continued treatment solely with clarithromycin. Her tongue returned to normal within 2 days of discontinuing moxifloxacin, and her right finger has shown no signs of recurrence for 12 months.
In conclusion, clinicians should be cautious of agents and lifestyle choices that can cause BHT, particularly moxifloxacin. To avoid patient anxiety or treatment changes, it is critical to counsel patients prior to such treatments.
Source: American Journal of Case Reports