A 35-year-old lady developed anorectal TB without any history of contact with a TB patient
She presented to the hospital with complaints of abdominal pain and bleeding from the rectum. She reported losing 7 kg weight in the past 9 months. There was no history of cough and she did not report having TB or any kind of contact with a diagnosed case.
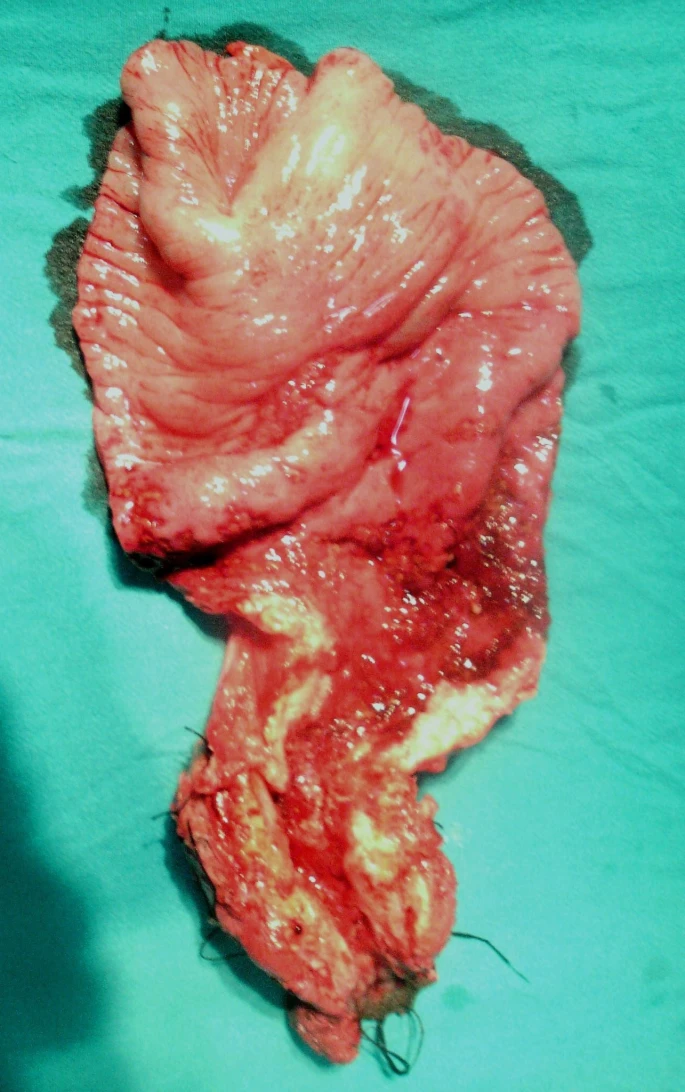
On examination, doctors found palpable masses in the lower abdomen. They then proceeded with the rectal examination which revealed stricture in the lower rectum. The mucosa bled easily when touched. On a contrast CT of the abdomen and pelvis, doctors confirmed the stricture. Moreover, they found a dilated and hypertrophied upper rectum on laparotomy.
Resection of the Tissue and Diagnosis
Doctors carried out an abdominoperineal resection. The resected specimen consisted of the lower rectum and upper anal region. The next step was to send it for a histological examination. Results revealed the presence of caseating granulomas in the tissue, a typical histological feature of TB. Moreover, the tissue showed signet-ring adenocarcinoma infiltrating the intestinal serosa. Based on these findings, doctors concluded a diagnosis of adenocarcinoma coexisting with anorectal TB.
Intestinal TB: What are the Odds?
Intestinal TB is uncommon accounting for only a small percentage of extra-pulmonary TBs. If at all, we only come across intestinal TB secondary to a pulmonary focus. The mechanism involves swallowing bacteria-seeded sputum or hematogenous spread by the organism. Anyhow, the manifestations are usually similar to other chronic GIT diseases like Crohn’s disease involving abdominal pain, bleeding, night sweats and palpable abdominal mass. Hence, a definitive diagnosis can become quite challenging especially when a person is negative for a history of TB or contact with a case.
Anorectal TB: Rare upon Rare!
When a person develops intestinal TB, it is usually the ileocaecal region that gets affected. We rarely see the involvement of the rectum in clinical settings. However, the patient under discussion developed anorectal TB, that too with a coexisting adenocarcinoma which makes this case even rarer.
The association between intestinal TB and adenocarcinoma at the same site is rather complex. Doctors propose various theories to untangle the complexity of their simultaneous occurrences. Only a few cases have been documented and doctors suggest that the association goes both ways. Intestinal diseases like ulcerative colitis, Crohn’s disease and intestinal TB etc. frequently garden malignancy. The reason lies in the fact that these diseases induce mucosal inflammation and damage. Most of the time, they instigate epithelial metaplasia and dysplasia which is followed by the development of adenocarcinoma. Clinicians have seen that people who develop pulmonary TB are at a greater risk for developing lung adenocarcinoma because of TB induced epithelial scarring. Thus, extrapolating this finding supports the aforementioned theory which advocates that TB induced mucosal damage can be a cause of coexisting intestinal adenocarcinoma.
Another popular belief that partly explains the association stems from the observation that people with malignancy are more prone to infections like tuberculosis. Malnutrition and weight loss associated with advanced stage neoplastic disease compromise host immunity. This leads to the reactivation of a latent infection. Hence, this school of thought suggests that the adenocarcinoma precedes and fuels the tubercular lesion. Whatever the aetiology may be, one thing that we know for certain is that anorectal TB in conjunction with intestinal adenocarcinoma requires intensive therapy. Moreover, it requires long term monitoring to look for relapse of both TB and cancer.
Treatment of Anorectal TB
For all kinds of TB, treatment begins with the typical anti-TB drugs. Doctors divide it into two phases. The first phase is an intensive phase in which all four drugs (or at least 3) namely rifampicin, isoniazid, pyrazinamide and ethambutol are given for 2 months. Whereas in the next phase called the continuation phase, doctors give isoniazid and rifampicin for 7-10 months.
WHO has recently launched DOTS (Directly Observed Therapy Short Course) guidelines for the treatment of TB patients. These guidelines bring a highly supervised therapy to the table in which the patient takes each dose in the presence of a healthcare worker or a responsible caretaker. It has shown to affect the disease prognosis significantly with those observing DOTS achieving much higher positive outcomes.
Patient’s Outcome
Doctors gave her adequate anti-TB therapy for six months. Additionally, she received chemotherapy with 5-fluorouracil and leucovorin for her intestinal cancer. The treatment worked out well. She turned out symptom-free at the end of one year.