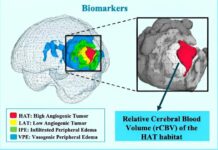
Glioblastoma is an aggressive brain tumor that occurs in the central nervous system (brain and spinal cord). It is difficult to treat and is usually fatal because of the way it invades vital brain tissue, surgeons may have to leave a part of it inside.
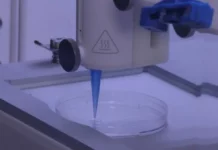
Now, the rise of 3D bioprinting has given scientists from Tel Aviv University a chance to study glioblastomas more closely. Previously, we reported that this approach has been taken to bioprint human organoids in order to study the effects of drugs before human trials and to study the in vivo organ’s development.
“If we take a sample from a patient’s tissue, together with its extracellular matrix, we can 3D-bioprint from this sample 100 tiny tumors and test many different drugs in various combinations to discover the optimal treatment for this specific tumor,”
– Cancer researcher, nanomedicine specialist, and study author Ronit Satchi-Fainaro.
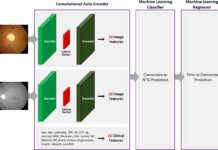
After harvesting the patient’s cells, which included tumor cells, astrocytes, microglia, the research team converted them into bioink. They printed the structures into a hospitable environment made from the same patients’ extracellular matrix. Finally, they harvested endothelial cells and pericytes from the patient and created a functional blood supply to ensure the cells’ survival.
Experimenting on a brain tumor
Although the 3D printed model worked, was it any different than just using glioblastoma cells in a petri dish?
They tested the two using a key protein found in glioblastoma: P-selectin.
In a previous study, the Tel Aviv team discovered that cancer cells produced P-selectin when they encountered the brain’s immune cells i.e microglia. The protein then encouraged the microglia to actually support the tumors growth instead of acting against it, as is the normal function of the immune system.
When they introduced a p-selectin inhibitor into both the lab glioblastoma culture and the 3D printed structure, they found that there was indeed a difference. The inhibitor did not diminish the protein’s function in the culture, as it would in vivo. In the 3D model, however, it actually worked.
“The reason is that cancer, like all tissues, behaves very differently on a plastic surface than it does in the human body. Approximately 90 percent of all experimental drugs fail at the clinical stage because the success achieved in the lab is not reproduced in patients.”
– Satchi-Fainaro
This experiment cements the fact that the team’s new 3D model is as close as researchers can get to studying the glioblastoma’s behavior. They believe that they can use the model to create personalized tumor treatment plans rapidly, ensuring a better outcome for glioblastoma patients.
Source: Science Advances
DOI: 10.1126/sciadv.abi9119
EurekAlert
https://www.eurekalert.org/news-releases/925555