Recent years have seen a huge boom in the pharmaceutical industry. As drug research continues to evolve and become more refined, these companies compete to create the best formula that can treat a targeted disease. The COVID-19 pandemic is no exception to this market. Various drugs have been produced to treat the viral disease’s symptoms since the beginning of 2020, a situation demonstrated by the many choices in vaccines we currently have.
What makes the process complicated is that companies do not create only one version of their targeted drug. Instead, they try various chemical combinations to find the perfect one. So how do they know which one works?
Drug companies and regulatory authorities like the FDA test medication using clinical trials. These usually begin with animal models. After clearing the initial stages, companies recruit human volunteers to try the drugs out and report back.
However, animal models don’t guarantee a safe human trial and there is always a risk of things going awry.
Tiny lungs
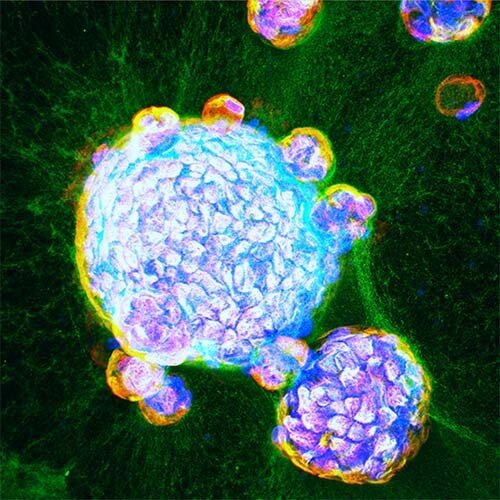
Scientists have been working to create tiny organoids (like these mini bioprinted pancreas) that can represent actual organs without any risk to life. These organoids are made of all the different types of tissues that exist in human organs so that researchers can comprehensively understand a drug’s effect on each type of cell.
Following the COVID pandemic, a team from the University of California San Diego School of Medicine has successfully engineered human lung organoids that can help improve initial drug testing.
LEAD CO-AUTHOR PRADIPTA GHOSH, MD, PROFESSOR, DIRECTOR OF THE INSTITUTE FOR NETWORK MEDICINE AND EXECUTIVE DIRECTOR OF THE HUMANOID CENTER OF RESEARCH EXCELLENCE (CORE) AT UC SAN DIEGO SCHOOL OF MEDICINE
“This human disease model will now allow us to test drug efficacy and toxicity, and reject ineffective compounds early in the process, at ‘Phase 0,’ before human clinical trials begin.”
The study, published in eLife, explains that the researchers took adult stem cells from lungs resected due to a tumor. They then supplied these cells with growth factors, enabling them to create an organoid that could represent both the upper and lower airways.
The team then infected these organoids with COVID-19 and observed that the virus initially doubled down on the upper airway, while the lower airway cells triggered the immune response. These insights will hopefully help advance COVID-19 treatment in the future.
A start
For now, the researchers have begun using the organoids for disease modeling and to test drugs.
SOUMITA DAS, PH.D., ASSOCIATE PROFESSOR OF PATHOLOGY AT UC SAN DIEGO SCHOOL OF MEDICINE AND FOUNDING CO-DIRECTOR AND CHIEF SCIENTIFIC OFFICER OF HUMANOID CORE.
“Our lung organoids are now ready to use to explore the uncharted territory of COVID-19, including post-COVID complications, such as lung fibrosis. We have already begun to test drugs for their ability to control viral infection—from entry to replication to spread—the runaway immune response that is so often fatal, and lung fibrosis”.
Source: UC San Diego
https://health.ucsd.edu/news/releases/Pages/2021-08-31-human-mini-lungs-grown-in-lab-dishes-are-closest-yet-to-real-thing.aspx