Case Report
Bayliss et al. first described Twiddler’s Syndrome 50 years ago. It is a very serious condition caused by the patient’s mechanical manipulation of the pacemaker generator. And can manifest without or with symptoms such as syncope, vertiginous disorders, fatigue, abdominal pulsation due to nerve stimulation, rhythmic arm movements due to brachial plexus stimulation, and chest pain (sometimes described as an intermittent “firing/shock in chest”). It can also kill the sufferer.
This report presents a case of a patient with Twiddler’s syndrome who was admitted to the neurological clinic due to a suspicion that the symptoms were neurological in nature.
Case Presentation
A 70-year-old female patient was admitted to the neurological clinic after experiencing recurrent presyncope and syncope, vertiginous disorders, headache, nausea, and vomiting. These symptoms began two months after the pacemaker was implanted, according to her anamnesis. A single chamber ventricular pacemaker was implanted with appropriate lead characteristics for sensing and pacing.
Her medical history was negative for coronary heart disease and neurological illnesses. The physical examination was ordinary, with a heart rate of 60 beats per minute and blood pressure of 150/80 mmHg. There are no auscultation abnormalities.
Investigations:
The first electrocardiogram (ECG) revealed a steady ventricular paced rhythm. The neurological examination was negative, but Romberg’s test came back positive. Because of the suspicion of a stroke, a computed tomography of the head was performed. Her CT scan showed no apparent pathomorphological abnormalities. Furthermore, an electroencephalogram was performed, which was normal.
After consulting with the cardiologist concerning additional treatment, the pacemaker interrogation was recommended and performed. It demonstrated an increase and instability in the capture threshold of the ventricular lead that began about 2 months after pacemaker placement.
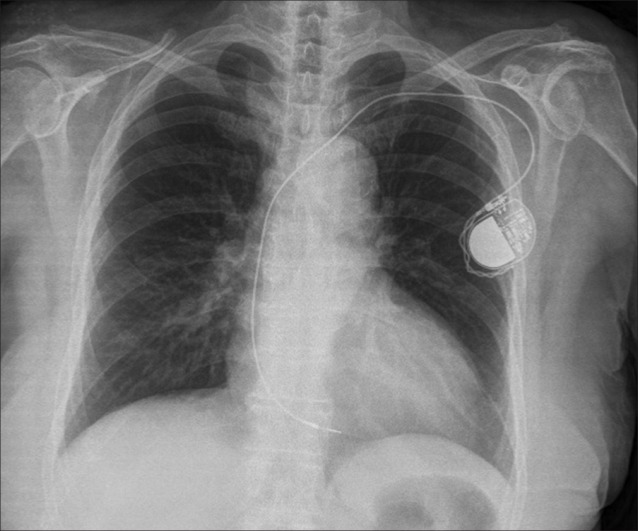
Another ECG strip was performed, and the intermittent failure of proper ventricular capture was noted. Furthermore, a chest X-ray was taken, which revealed the displacement of the ventricular lead in the right ventricle with a twisted lead near the generator. Pacemaker Twiddler’s Syndrome was diagnosed. She was promptly brought to the catheterization lab, where the new screw-in ventricular lead was implanted. The generator and fresh lead were secured beneath the pectoral muscle with a nonabsorbable suture.
Following the intervention, the patient stated that she did not alter the pacemaker. But her son stated that she was experiencing mental health issues at the time and was really unhappy. Two days later, after consulting with a psychiatrist, she was released from the hospital without incident.
Discussion
Twiddler’s syndrome is a relatively rare complication after pacemaker implantation, with a frequency of 0.07%-7%, and is primarily caused by patient tampering with the pacemaker generator. Manipulation with the generator causes dislocation and/or breakage of the leads. This syndrome typically appears in the first year following implantation, as in our case, but it might occur later. It is not limited to cardiac devices; it can also occur with central venous catheters. Twiddler’s syndrome is especially harmful in defibrillator patients because it can result in erroneous treatment of malignant ventricular arrhythmias and inappropriate shocks due to a lack of proper sensing and capture.
Fast diagnosis and treatment is critical. The ECG, chest X-ray, and pacemaker interrogation can all offer us with the information we need, and they should be considered conventional diagnostic techniques for Twiddler’s syndrome. Chest X-rays provide an excellent visual of the lead coiling and device rotation. Remote monitoring and follow-up, including automatic alarms for arrhythmias and changes in pacemaker fundamental parameters, can also provide valuable information concerning the cardiac device’s malfunction.
There are two critical factors to consider while determining how to prevent Twiddler’s syndrome. The first is that the patients who are candidates for pacemakers are not all the same, and that Cardiologists should pay attention to high risk patients for the development of Twiddler’s syndrome: female, elderly, and obese patients, pediatric patients, patients with mental disorders, and patients who are at risk for psychoorganic syndrome.
And second fact is education about life with pacemakers and similar devices is crucial for patients and families. Mismanaged devices can be dangerous, leading to syncope, neurological symptoms, and potentially fatal cardiac arrhythmia. Medical staff should provide comprehensive information on pacemaker usage and care.