From urinary tract infection to septic shock during pregnancy in a 20-year-old woman at 24 weeks of pregnancy!
A 20-year-old African-American woman, G2P1001, presented to the emergency department at 24 weeks and 2 days of gestation with complaints of generalized lower back pain, dizziness, chills, malaise, and increased urinary frequency for the past 1 day. The patient had received no prenatal care and had not gotten any antenatal ultrasounds.
On examination in the emergency department, the patient was alert and oriented. She was pyrexic with a temperature of 102.4 ℉, a blood pressure reading of 104/54 mmHg, pulse rate of 127 bpm, and respiratory rate of 24.
Physical examination revealed no abnormality. There no costovertebral or abdominal tenderness. A STAT urine dip was not consistent with a urinary tract infection. Urinalysis was negative for nitrites, with only trace leukocyte esterase and blood; bacteria and white blood cells were not measured. White blood cell was 23.9.
After collecting a urine sample for urine culture, and a blood sample for cultures and lactate levels, the patient was started on empiric Ceftriaxone 1g intravenous daily and maintenance fluids. She was given a total of 2 L of bolus fluids.
Although there were no prenatal visits, there was a history of a visit to the emergency department for nausea and vomiting around 3 months back with a documented diagnosis of urinary tract infection. During that visit, the urinalysis had shown positive nitrites, many bacteria, pyuria, trace leukocyte esterase; and urine culture had grown E. coli. The patient was advised to be treated on an outpatient basis with Cephalexin, but she never bought the antibiotics.
On the second day of current hospital admission, the urine culture again grew E. coli. The lactate levels were physiologic, and the patient was continued on the Ceftriaxone and maintenance fluids.
The patient improved only minimally despite adequate fluids and antibiotics. A day later, the patient’s condition deteriorated further with acute distress, worsened tachycardia up to 140 bpm, worsened fever up to 104.1 degrees ℉, increased respiratory rate near 40. Despite fluid bolus, the patient’s hypotension didn’t improve. Eventually, her breathing became labored despite 100% oxygen on pulse oximetry. A chest X-ray showed no acute processes.
A working diagnosis of septic shock was made, and the patient was shifted to the medical intensive care unit.
In the medical intensive care unit, Ceftriaxone was discontinued. Instead, she was started on Piperacillin/Tazobactam and stress-dose steroids.
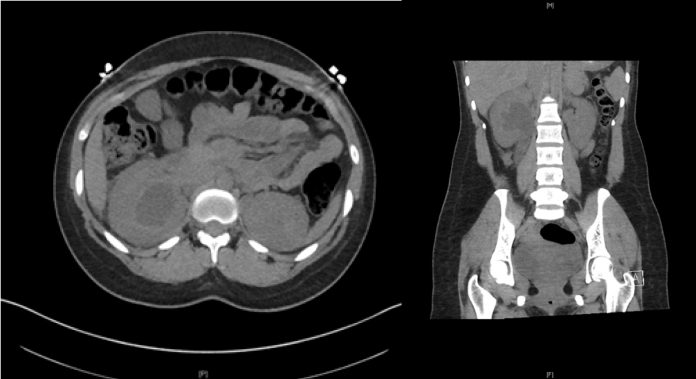
A renal computerized tomography scan was performed, which showed severe right hydronephrosis with perinephric and peri-ureteric fat stranding with no obstructions. An ultrasound was also performed.
The findings of both the CT scan and the ultrasound were consistent with a diagnosis of right pyelonephritis.
On 3rd day of hospital admission, she was started on vasopressors in the medical ICU and was then transferred back to labor and delivery.
The patient was stabilized by then. Her blood cultures were negative at 48 hours.
The patient had improved substantially, so she was discharged with the advice of close outpatient follow-up and a prescription of Cephalexin for the remainder of her pregnancy.



