- Autoimmune encephalitis causes memory loss, confusion and psychosis.
- The condition is more common in young females, especially with ovarian teratomas.
- This is the case of a 28-year-old male patient without any malignancies with a rare case of NMDA encephalitis.
A 28-year-old male patient presented with restlessness, hallucinations, confusion and bizarre behaviour with a history of 2 days. The patient’s medical history revealed that he had stroke with left sided facial droop, stroke and seizure disorder. His family did not have a history of any psychiatric disorders. According to his family, he had no recent history of loss of weight, loss of appetite, urinary symptoms, headaches, cough, sore throat, runny nose, vomiting, nausea, chills and fever. Physical examination showed that he was afebrile and hemodynamically stable. He was diagnosed with NMDA encephalitis.
Examination
Examination further showed that he was alert and oriented to person and place. Although, disoriented to time. In addition, according to his fiancé he had been hearing voices, acting paranoid, pacing around the room and not sleeping. He was admitted to the psychiatry department for acute psychosis and prescribed valproic acid, risperidone, and benztropine, with haloperidol and diphenhydramine. Although, he did not show any improvements.
He was admitted for acute psychosis twice before and discharged with recommendation of outpatient follow-up. The patient did not show up for any follow-ups, therefore, no workup was done. Similarly, his mental status worsened and he continued to be unresponsive to medications.
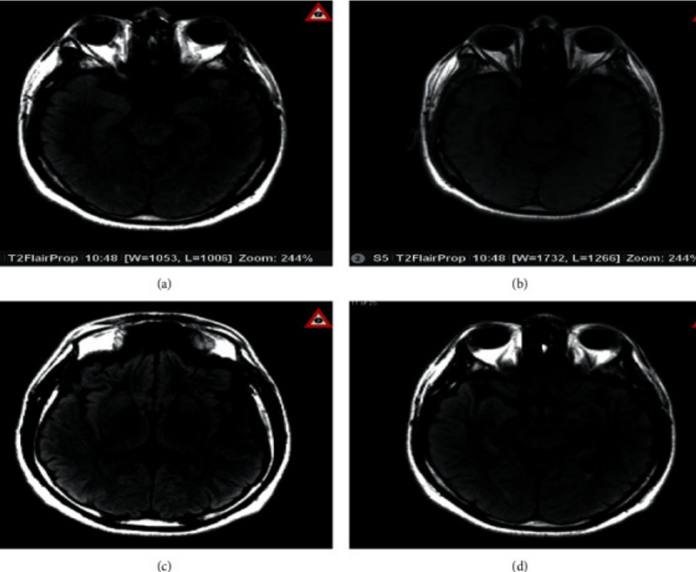
For further evaluation, doctors advised magnetic resonance imaging (MRI) of the brain with contrast, lumbar puncture (LP), and an autoimmune workup. Brain MRI showed areas of bright signal intensity throughout the brain parenchyma most notable in the bilateral insular cortices and medial temporal lobes, consistent with encephalitis. Oligoclonal bands were positive in the blood and CSF.
Initial management included empirical treatment with vancomycin, ceftriaxone, and acyclovir for infectious causes of encephalitis. In addition, NMDAR antibodies in the CSF confirmed the diagnosis. The empiric antibiotics and acyclovir were discontinued. Moreover, the patient was treated with intravenous immunoglobulin 400 mg/kg/day and methylprednisolone 1g/day for 5 days.
The patient showed a significant improvement in symptoms after treatment. He was seen having more meaningful conversations with improved speech. The patient was discharged with outpatient follow-ups.
References
Finding the Cause of Psychosis: A Challenging Case of Anti-NMDAR Encephalitis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7578717/



