Case of pseudofungi in elderly black breast cancer and covid-19 patient.
This article describes the case of pseudofungi in an elderly black male patient with history of breast cancer and covid-19. The patient with invasive ductal carcinoma presented to the emergency with several days history of bleeding from the left breast because of fungating breast cancer.
Examination
Laboratory results of the patient revealed anaemia with a normal white blood cell count and absolute neutrophil count. The patient was also diagnosed with bilateral pulmonary embolism (PE) that caused lung infarcts in the right middle and left lower lobes twenty days ago. The events followed a covid-19 infection that caused bilateral interstitial pneumonia that was complicated by sepsis. The patient’s condition was complicated because of sepsis. Doctors advised treatment with hydroxychloroquine and azithromycin.
In addition, the patient’s neoadjuvant chemotherapy with paclitaxel had to be delayed for 3 weeks because of the acute infections. He was further referred for surgical management because of concerns of disease progression.
Treatment
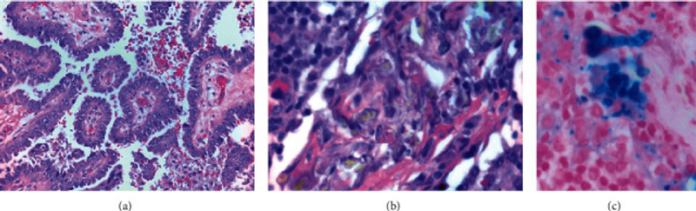
The patient received a left-modified radical mastectomy with partial excision of the pectoralis major muscle and axillary lymphadenectomy. Pathology after mastectomy revealed a mass, measuring 15 cm fungating through the skin. It further showed papillary architecture with nuclear pleomorphism. In addition, 11 out of 28 lymph nodes were positive for malignant involvement. Two of the lymph nodes also demonstrated subscapsular and intrasinusoidal refractile birefringent crystal like structures. Staining with hematoxylin and eosin suggested an Aspergillus infection. There were no signs of necrotising granulomas in any lymph nodes. However, areas of foreign body giant cell reaction and extensive hemosedrin pigment deposition were present.
Initial treatment included two doses of voriconazole. The patient also underwent multiple diagnostic tests including CXR, CT, chest and sinus UA, aspergillosis galactomannan, fungal blood cultures, and procalcitonin. The tests were all unremarkable. He had no other symptoms. In addition, the antifungals were discontinued after ruling out true mycosis and the patient’s anticoagulation status was balanced. The patient remained afebrile and showed no other symptoms of infection in the weeks that followed.
References
Pseudofungi in an Immunocompromised Patient with Breast Cancer and COVID-19 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7599402/



