Case Report
Hydatidiform mole is a benign gestational trophoblastic disease (GTD) that exists in two forms: total and partial. Molar pregnancy occurs in around 1-2 out of every 1000 deliveries, with Asians having the highest prevalence.
The diagnosis and follow-up of patients with molar pregnancy are critical. Because there have been cases of progression from molar pregnancy to invasive mole and choriocarcinoma.
Partial molar pregnancy is typically diagnosed as a missing or incomplete miscarriage in the first trimester of pregnancy.
A molar pregnancy coexisting with a live molar pregnancy fetus is extremely unusual, accounting for about 0.005-0.01% of all pregnancies. It also poses some dangers to the mother and the fetus. The most common risk factor is preeclampsia.
Many pregnancies are unable to continue due to fetal triploidy, severe intrauterine growth restriction, and poor placental function. If the molar pregnancy persists, its care is tough.
A uncommon incidence of partial hydatidiform molar pregnancy with a viable fetus at 5-6 lunar months of pregnancy is being presented.
Case Presentation
A deceased fetus and placenta from a normal vaginal delivery (NVD) arrived at Shahid Mohammedi Lab Hospital. This deceased fetus was the result of a 21-year-old Persian woman’s first pregnancy, grouped o+, with no significant medical history and routine prenatal check-ups.
The fetus weighed 150 g and had no major abnormalities, with external genitalia compatible with the male gender. His crown-rump length (CRL), crown-heel length (CHL), and head circumference (HC) measures were 15, 26, and 18.5 cm, respectively. That corresponded to 5-6 lunar months of pregnancy. All internal organs were present in a Y incision of the chest and abdomen, with no obvious anomalies, and tissue collection from all organs was performed for histology. The placenta was entire with an attached umbilical cord, measuring 18 × 16 × 3 cm and weighing 600 g.
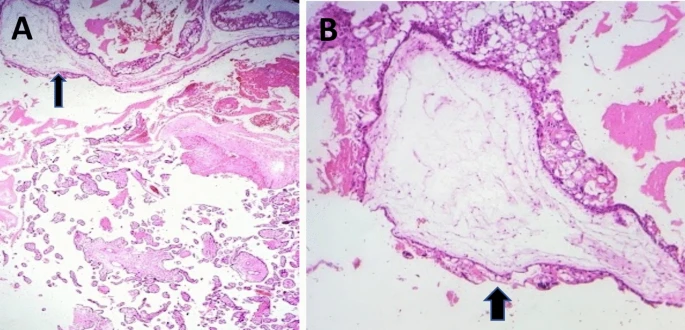
The placenta had multiple grape-like vesicular cystic formations with hemorrhagic parenchyma, which was consistent with molar pregnancy. The umbilical chord was grossly normal, with a central insertion and three vessels on its cross-section. Microscopic examination of hematoxylin and eosin (H and E) stain slides obtained from fetal tissue sampling revealed no major pathological abnormalities.
Microscopic examination of the placenta revealed enormous hydropic villi with cistern development, scalloping. And peripheral trophoblastic proliferation, interspersed with normal and tiny villi, as well as fibrotic villi consistent with partial molar pregnancy.
Discussion
Hydatidiform mole is a benign gestational trophoblastic disease (GTD) that exists in two forms: total and partial. Complete molar pregnancy has a diploid karyotype. But partial molar pregnancy has a triploid karyotype (69 XXY, 69 XXX, and 69 XYY) due to the fertilization of one ovum by two sperms. Hydatiform molar pregnancy with a viable fetus is classified into three types: the most common is twin pregnancy with one normal fetus and one full mole. The second is a twin pregnancy that includes one normal fetus and a partial mole. The third is a partial mole with one normal fetus, which is an uncommon form. Our case is the third type.
If the fetus is triploid, it will not survive birth due to several abnormalities and severe intrauterine growth retardation caused by poor placental circulation.
The incidence of hydatidiform mole is high in women under the ages of 20 (10.52/1000 births) and 39 (5.95/1000 births).
The probability of molar pregnancy increases to 2 in 10,000 pregnancies due to assisted reproductive technologies (ART), such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI).
Patients with molar pregnancies may experience a variety of symptoms, including vaginal bleeding, a big uterus, abdominal pain, nausea, vomiting, hyperthyroidism, hypertension, and proteinuria. Serum levels of β-HCG (human chorionic gonadotropin) are significantly raised in laboratory settings. Our client did not exhibit these symptoms and had no prior medical or surgical history.
It is critical to diagnose and monitor people with molar pregnancy because there have been reports of progression to invasive mole and choriocarcinoma.