This article describes the case of a 21-year-old who presented with a non-tender lump in her left lower neck. The patient’s medical history did not show any significant findings. She was both clinically and biochemically euthyroid. Doctors advised a thyroid ultrasound for further evaluation which showed a solitary large solid-cystic nodule in the left lobe-isthmus. However, there were no signs of cervical lymphadenopathy. Whereas fine needle aspiration cytology (FNAC) of the nodule yielded haemorrhagic contents. Based on the investigation findings, this was a case of mummification of benign thyroid nodule.
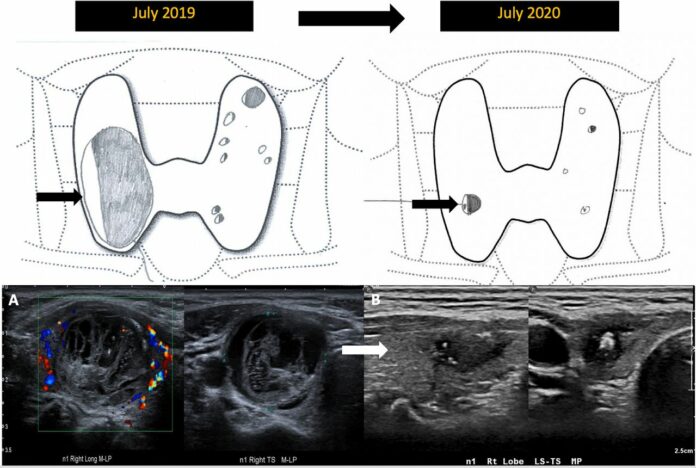
For the next 3 years doctors followed the nodule via an ultrasound. The findings showed a progressive shrinkage of the nodule’s cystic portions with calcification an content replacement with iso-to-hypoechoic contents. Doctors suspected for the nodule to be malignant, therefore, classified it as a TR-5 nodule based on he thyroid imaging reporting and data system (ACR-TIRADS).
FNAC was repeated on the solid portions which showed non-diagnostic acellular contents. The most recent follow-up showed that the nodule continued to decrease in size with degenerative changes.
The findings were consistent with benign mummification of the thyroid nodule.
Over time, benign thyroid nodules are known to undergo mummification and degeneration. This is either spontaneous, because of percutaneous ethanol or laser ablation, following FNAC or due to cystic portions becoming desiccated. The vascular supply is disrupted in mummified solid components which results in intranodal hypoxia associated with haemorrhage and scarring.
The mummified thyroid nodule typically presents as necrosis associated with posterior shadowing, avascularity and shrinkage. In addition, it also presents as a subcapsular granulation tissue with peripheral black and white halos. In some cases the mummification can mimic malignancy.
According to the study, mummified nodules may demonstrate irregular ill-defined nodule margins due to capsular collapse, taller-than-wide shape from asymmetric fibrous healing with transverse shrinking, replacement of cystic contents with iso-to-hypoechoic ‘solid’ contents due to fibrosis and internal echogenic foci attributed to dystrophic calcifications or colloid material, usually seen in later stages. Nodule shrinkage, a key feature of mummification, may rarely be seen in papillary thyroid carcinomas.
Therefore, it is important to distinguish mummification from malignancy. The case iterates the importance of reviewing prior comparison imaging for morphological changes and shrinkage.
References
Mummified thyroid nodule: a diagnostic and management conundrum https://casereports.bmj.com/content/14/5/e242238



