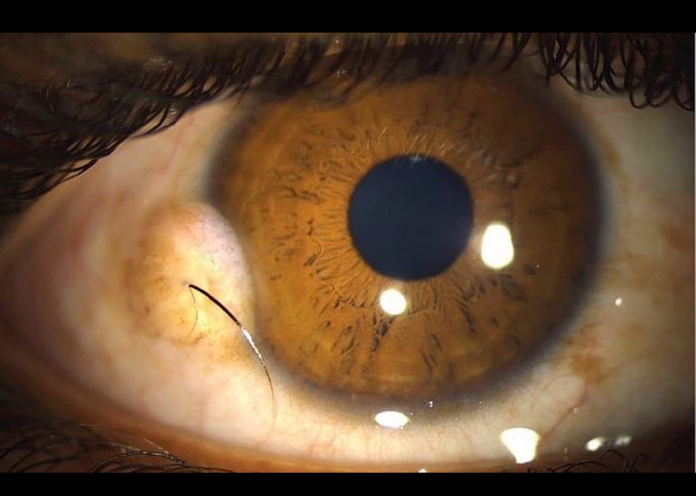
The picture attached above shows a mass in the right eye of a teenage boy. The mass was diagnosed to be a limbal dermoid which has been gradually increasing in size since his childhood.
Limbal dermoid has an
incidence of 1 to 3 cases per 10,000 people. It is normal, non-cancerous
overgrowth of tissue at an abnormal location, where it is not to be present
normally, usually since birth. In other words, it is a benign congenital tumour containing choristomatous tissue, including connective tissue,
sweat glands, fat, hair, teeth, muscle or virtually any tissue type. Chances of
it having malignant potential are extremely scarce.
The most common site is the inferior temporal quadrant of the corneal
limbus. Though present since birth but may take a decade or two to be diagnosed,
usually by the age of 16 years, as it increases in size as the body grows.

Source: https://emedicine.medscape.com/article/1195334-overview#a6
The affected child may complain of decreased vision, gritty sensation, cosmetically displeasing and an enlarging mass in the eye. This fleshy, yellowish-white mass may have hair plunging out from it or superficial fine network of capillaries running over it.
When the case in discussion here was examined, an elevated yellowish mass occupying 7 to 9 o’clock position in the right eye along the limbus was revealed. Two hair follicles and fine vessels were also observed over the lesion.
Does it affect the vision?
Vision may be affected if the visual axis gets obstructed by the mass, either due to the infringement of the lesion or lipid infiltration or astigmatism, thus secondarily affecting the vision. The cornea or sclera may perforate if staphyloma forms.

Source: https://www.researchgate.net/figure/Grade-III-dermoid-with-staphyloma_fig3_236193456
Limbal dermoid may be associated with other syndromes, therefore a thorough history and examination are essential in all cases. Having said that, limbal dermoid, per se, doesn’t require laboratory support (not even biopsy) to establish a diagnosis i.e. the diagnosis is clinical. Imaging may only be necessary if the mass is suspected to be affecting other ocular tissues/muscles and if surgery is being considered.
Treatment options are variable:
– Topical lubrication to relieve the gritty sensation
– Periodic removal of irritating cilia
– Lesion excision for cosmesis purpose or vision
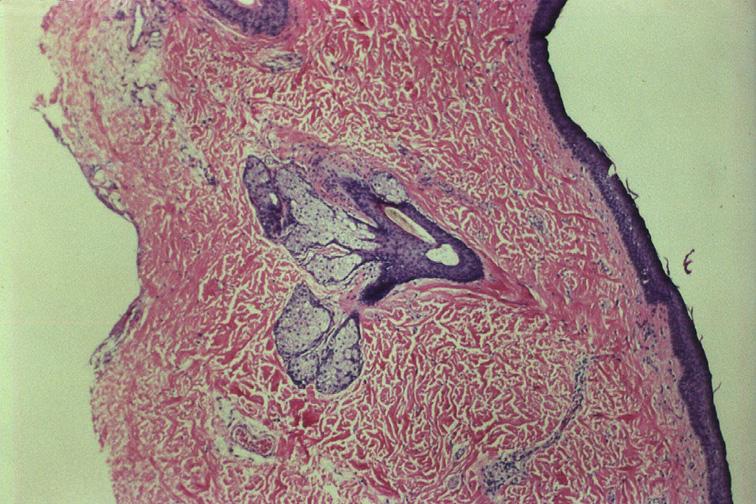
Superficial sclerokeratectomy is the procedure of choice. Excised tissue should be sent for histopathology for a definitive diagnosis. Having said that, when opting for surgical removal, the benefits of excision should be weighed against the adverse effects of surgical scar formation.
The boy in the above-mentioned case underwent lamellar keratectomy, the excised tissue was sent for a biopsy which confirmed the diagnosis.
Source: https://emedicine.medscape.com/article/1195334-overview#a6
References
Sherman, M. D. (2018, September 25th). Limbal Dermoid. Retrieved from Emedicine. Medscape: https://emedicine.medscape.com/article/1195334-overview#a6
Pirouzian, Amir. (2013). Management of pediatric corneal limbal dermoids. Clinical ophthalmology (Auckland, N.Z.). 7. 607-14. 10.2147/OPTH.S38663.