Only 0.1% of cases of Mycoplasma pneumoniae infection present with neurological impediments. Although direct intracerebral infections are possible in these patients, autoimmune-mediated reactions to molecular mimicry are very common pathophysiology. The complications are peripheral neuritis, for example, Guillain-Barre syndrome, immune-mediated encephalitis and many others.
Case Report
Miller Fisher syndrome is a variant of Guillain-Barre syndrome, which is rarely has a link with Mycoplasma pneumonia infection. This case is of a patient with Miller Fisher syndrome with Mycoplasma pneumoniae infection.
She had no known medical conditions and presented with double vision, in addition to body imbalances for two days. According to her, the onset of diplopia was sudden, painless, and looking in a specific direction wasn’t a cause. Furthermore, she swayed to her right side with a preceding history of fever and mild flu for 5 days.
She also complained of bilateral numbness and cramping over the hands and feet since the day before the presentation. However, there was no stiffness in the neck, weakness in the upper and lower limbs, slurring of speech, dyspnea, and dysphagia.
Examination
Upon physical examination, she had bilateral diplopia over the lateral gaze with no other abnormal findings. Although Romberg’s test was negative, sharpened Romberg’s test was positive. All other investigations were also normal.
Doctors also did a CT scan, which revealed no space-occupying lesion or intracranial bleeding. Moreover, her nerve conduction study showed mild sensory axonal polyneuropathy in addition to segmental demyelination. Moreover, there was a bilateral absence of H reflex.
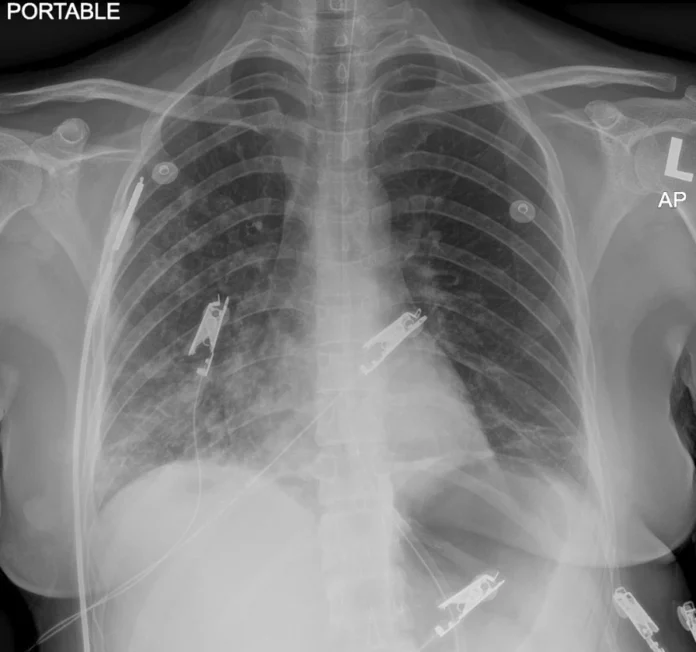
Due to the presence of ataxia and diplopia, doctors suspected it to be the Miller Fischer syndrome variant of Guillain-Barre syndrome. The confirmation was through the presence of serum anti-GQ1b autoantibody. They started her on IV immunoglobulin once daily. However, on the second day, she developed SOB and a worsening cough. Chest radiography revealed homogenous opacity over the lower right zone. So, the doctors started her on IV co-amoxiclav thrice daily, which was escalated to IV piperacillin-tazobactam. But, after two days there was no improvement.
Susception of Atypical Pneumonia
Since the doctors suspected atypical pneumonia, Mycoplasma pneumonia antigen was taken, which was positive for 1 over 2560 titer of total mycoplasma antibody and presence of IgM antibody. Suggesting an acute infection, she was put on macrolide antibiotic azithromycin orally once daily for five days. In addition to the IV antibiotics given previously and IVIg treatment. Moreover, she also did inpatient therapy for some days before discharge.