Case Presentation
A 29-year-old man presented to the emergency department with a complaint of a seizure. Additionally, he complained of pain in the left leg one day ago. Furthermore, he was a known case of mitral valve prolapse, which was diagnosed when he was 18 years old. He was also a commercial airline pilot, and his working days were 18 days in one month. According to the patient, he was living in a high-altitude city. His family history included a first cousin with epilepsy. The doctors ordered a CT scan of the head, which was unremarkable. Therefore, he was referred to neurology.
The neurology department ruled out epilepsy as the cause of seizures. This is because EEG had turned out normal.
Presentation to the Emergency Department Again
One week after his initial presentation and referral to neurology, the patient presented again with pain in the left leg and shortness of breath. The doctors did not order any baseline blood investigations or any imaging. The doctors diagnosed him with a case of allergies and discharged him. In the following month, he experienced another seizure in the morning, for which he did not seek any medical care. He consulted a neurologist again, and they prescribed him levetiracetam.
Two months later, the patient presented to the emergency department again with shortness of breath, hemoptysis, left leg pain and left midsternal chest pain. The patient gave a history of travel for around 20 hours, two weeks before the presentation. His vitals were BP 145/88, MAP 107 mmHg, temperature 97.8 °F, HR 93, RR 16, and SaO2 of 95%. Physical examination revealed normal lung breath sounds, heart sounds and normal peripheral pulses. The doctors found no oedema and his neurological examination was normal. They ordered baseline investigations and imaging. The patient’s d-dimer levels were elevated. Chest CT scan with IV contrast revealed a bilateral pulmonary embolism and a 4mm lingular nodule. Therefore, the doctors administered IV tPA and oncology workup for the lingular nodule.
Diagnosis: May-Thurner Syndrome
The oncology workup and blood workup turned out negative for any malignancy or any other disease. Moreover, a full body CT scan revealed a diagnosis of May-Thurner Syndrome. This differential was given due to the symptoms he presented with.
Management
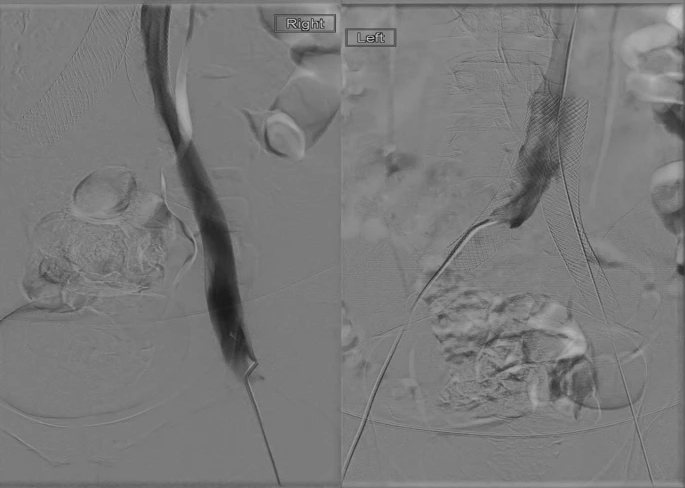
Thus, the doctors started discussing treatment options with the patient which included long-term medication for anticoagulation or surgery (venoplasty). The patient expressed his wish to choose the definitive management option, that being endovascular venoplasty with stent placement. The patient was referred to International Radiology, where radiologists placed stents in bilateral common iliac and right external iliac veins. After the stent placement, a CT scan was performed which showed the 3D placement of the stent and patent blood flow through the veins.
Follow-up
After this intervention, the doctors referred him to haematology for follow-up. 4 weeks after the venoplasty, the doctors switched him from heparin to aspirin. Six days after heparin was discontinued, the patient experienced leg pain again which indicated a thrombotic event, along with shortness of breath. His CT scan revealed a pulmonary embolism for which he was referred to interventional radiology.
The IR department performed a thrombectomy of the left popliteal vein through the left iliac veins and into the inferior vena cava and from the right external iliac vein into the inferior vena cava.
After this procedure, two 20 cm catheters were inserted bilaterally. tPA infusion was commenced through both catheters. After 24 hours, a fluoroscopy was performed which revealed that the treated segments of veins were patent. He was retained in the hospital for 24 more hours and was discharged after monitoring on apixaban as prophylaxis. There were no reported complications after this procedure.
On long-term follow-up, the patient reported no seizures, thrombotic events or presentation to the emergency department. The doctors found no positive testing for any coagulation disorders. However, the patient remains on Coumadin for life for the prevention of any coagulation events. The underlying reason for his seizures was attributed to the hypoxia caused by thrombotic events.
May-Thurner Syndrome (MTS)
May-Thurner Syndrome is a vascular disease which is caused by the right common iliac artery compressing the left common iliac vein against the lumbar spine, which eventually leads to deep vein thrombosis in the lower legs. This is most commonly seen in the left leg and is often diagnosed in females as compared to males.
Risk factors for having MTS include female sex, multiparity, oral contraceptives, scoliosis, dehydration, hypercoagulable disorders, and radiation exposure. Although, it is a rare case of deep vein thrombosis.
It presents with discolouration of the skin on the legs, swollen leg veins, throbbing and tenderness in the leg along with a feeling of heaviness.
May-Thurner Syndrome is diagnosed based on history along with imaging such as CT scans, MRI, Ultrasound, and venograms.
It is managed based on the symptoms and signs that the patient presents with. This includes procedures such as angioplasty and stenting and bypass surgery. After these interventions, medications such as anticoagulants or vena cava filters have to be used in order to prevent future thrombotic events.