- Chromosomal deletion syndromes are a class of diseases caused by the non-occurrence of parts of chromosomes
- Examples of such deletion syndromes include DiGeorge (22q11 – which causes cleft palate), Prader-Willi, Angelman, 5p cri du chat, and De Grouchy syndromes.
- The genetic diseases manifest as a variety of symptoms that may affect one’s mental or physical capabilities
- These symptoms may inhibit daily life activities including oral hygiene practices and dental treatments, therefore patients with such diseases need special dental care practices
De Grouchy Syndrome
De Grouchy syndrome occurs due to a long arm (q) deletion mutation in the 18th chromosome. Its prevalence is 1 in 40,000 live births, of which, only 6% of mutations are hereditary. Physically, the syndrome manifests as neurological deficiencies such causing mental retardation, delayed cognitive abilities, hormonal or IgA deficiency, genitourinary malformations, cardiac malformations, and limb anomalies such as foot hypotonia. Craniofacial abnormalities may also occur, which include brain anomalies, cleft lip/palate, prognathism, midface anomalies, cofosis (hearing loss), and anomalies of the auditory organ.
The report explains that growth hormone deficiency commonly causes mandibular retrusion and increased length of the lower 3rd of the face. Such orofacial abnormalities may affect dental eruption patterns, causing malocclusion and tooth crowding due to a lack of space. These conditions increase the chance of bacterial accumulation while making hygiene maintenance such as brushing or flossing, difficult to perform.
Medical History
This case outlines the treatment for an 8-year old patient with De Grouchy syndrome who presented to the Paediatric Department of the A.O.U San Giovanni di Dio and Ruggi D’Aragonna Hospital in Italy with a complaint of dental pain and difficulty in feeding.
The patient was referred to the hospital’s Department of Dentistry and Oral Surgery where a physical examination was conducted. Due to the patient’s syndromic mental retardation, he was ‘uncooperative’ during the physical exam, as reported in the case study.
The doctors report that the patient’s oral hygiene was poor, which caused inflamed gingiva and bacterial plaque accumulation. While there was no tooth mobility, a carious lesion affected the deciduous mandibular right second molar. The patient also had a short lingual fraenum which restricted his tongue movements.
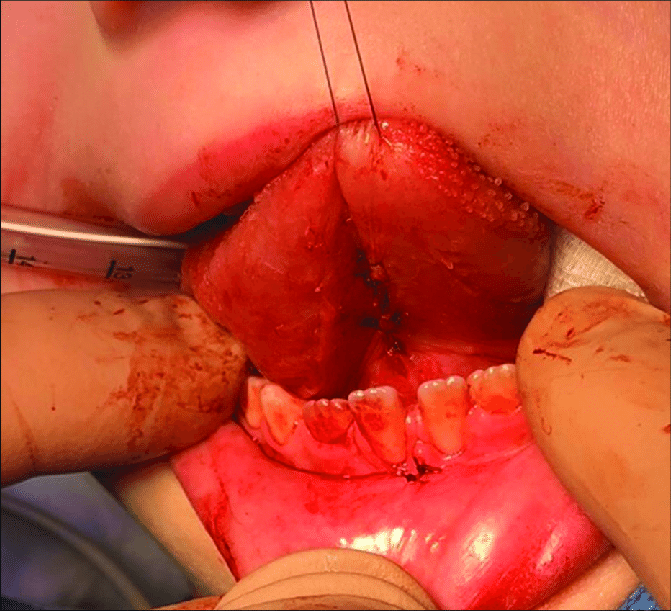
Upon discussion with a speech therapist, the team decided to perform lingual and lower labial frenectomies to improve tongue mobility. This would prevent symptoms related to ankyloglossia – including atypical swallowing patterns and inhibited mandibular growth- from occurring in the future.
The Treatment
The clinical team chose tooth extraction procedure, as it has a better chance of success in place of conservative treatment. Similarly, the frenectomies (i.e. complete removal of the frenulum), while invasive, guaranteed better results and lower recurrence as compared to the more conservative frenulectomy procedures.
According to the case report, syndromic diseases such as De Grouchy’s fall under “Disablement pertinent to dentistry”, which cause poor oral hygiene and non-compliance during dental procedures. These reasons result in frequent dental lesions and difficulties in treating them due to a non-cooperative or anxious patient. Therefore, such patients are usually treated in hospital settings under general anesthesia.
In the report, the doctors explain that while general anesthesia is a relatively safe procedure nowadays, it is not always free of complications. General anesthesia related mortalities occur with at a rate of 1 in 40,000, usually due to halothane gas, a common component in the drug mixture. Cardiac and respiratory complications may also occur and there is scarce literature available on the safety of repeated general anesthesia use for special needs patients. Therefore, the doctors planned a single surgery under general anesthesia for all 3 treatments so that the patient didn’t have to go through general anesthesia preparations again.
The doctors first performed an atraumatic deciduous tooth extraction. They controlled the bleeding using a buccal infiltration of local anesthetic with vasoconstrictor properties. After suturing the wound with a resorbable 5/0 vicryl thread, they performed the two frenectomies using an electric scalpel that aided cauterization. Again, local anesthesia infiltration helped prevent excessive bleeding. This was an important aspect of surgical planning, as the oral cavity is highly vascularized, therefore achieving hemostasis was critical. The authors recommend dental lasers as an alternative to the electric scalpel, as they are less invasive. Finally, the doctors used the same resorbable suture to close the wound so that the patient didn’t have to return for removal.
Prognosis
2 months later, an examination revealed that the wounds were healing well and lingual mobility and feeding had improved. The team referred the child to a speech therapist for functional rehabilitation. His parents were also instructed to help him maintain his oral hygiene to prevent further problems.
According to the authors, there is scarce literature available on the dental management of long arm (18 q) deletion syndrome. While they performed the treatments according to the criterion standard, they recommend that evidence based guidelines should be created for clinicians regarding the correct management of patients with the disease.
Reference
Pisano, M., Sangiovanni, G., D’Ambrosio, F., Romano, A., & Di Spirito, F. (2022). Oral Care in a Patient with Long Arm Deletion Syndrome of Chromosome 18: A Narrative Review and Case Presentation. The American journal of case reports, 23, e936142. https://doi.org/10.12659/AJCR.936142