Relapse of glioblastoma is very common and it usually takes just a few months after treatment for the initial brain tumour to recur. Hence, the survival rate of glioblastoma is 25% at one year and 5% at five years. Moreover, one of the most common challenges surgeons face is that they cannot always remove the tumour or the glioma stem cells linger in the brain completely.
Assistant Professor Quanyin Hu, University of Wisconsin Madison School of Pharmacy said,
One characteristic of glioblastoma is that the tumour cells are very aggressive, and they will infiltrate the surrounding tissues. So the surgeon can’t clearly feel the boundaries between the tumour and the normal tissue, and you cannot remove as much as possible because all the tissues in the brain are extremely important—you certainly don’t want to remove too much.”
He also said that relapse can happen each time after treatment, which decreases the rate of survival.
Immunity-Boosting Post-Operative Treatment
Hu’s CIPT Lab has formulated a powerful immunity-boosting postoperative treatment, which can combat the odds of patients with glioblastoma. The research about the treatment used on mouse models of human glioblastoma was published in Science Translational Medicine.
Hu said that they hope to prevent the relapse of glioblastoma. He further quoted,
We prove that it can actually eradicate these glioma stem cells, which can eventually prevent the glioblastoma from coming back. We can significantly improve survival.
Injectable Hydrogel
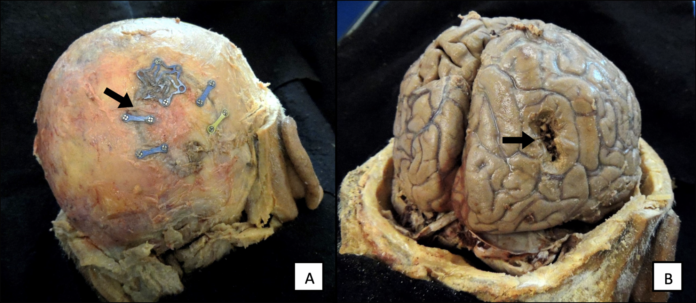
The lab developed an injectable hydrogel, which can be injected into the cavity that the excised tumour leaves behind. This delivery method shows a positive result because it fills the cavity of the brain completely, releasing medication into the tissues surrounding it. Moreover, it promotes a cancer-killing immune response.
The hydrogel consists of nanoparticles, which enter and reprogram some types of immune cells. These immune cells are called macrophages and usually clean the infectious invaders in the body. However, in a tumour environment, the immune system is suppressed and cancer growth is promoted. Furthermore, because of post-surgery inflammation, these macrophages move to the surgical site causing a relapse.
Hu said,
We want to take advantage of these macrophages and turn them from enemy to ally
For the macrophages to become an ally, the nanoparticles can engineer the macrophages, targeting CD133 glycoprotein, which is a market for cancer stem cells. The team also added that the CD47 antibody signals the promotion of macrophages to recognize cancer cells. The preclinical results were successful and generated glioma stem-cell-specific chimeric antigen receptor macrophages. It is engineered to target and eventually kill any glioma stem cells left behind.
If this is effective in humans, the need for chemotherapy and radiation after surgery can be eliminated. In addition, the toxic side effects will also be catered to this way.
Hu said,
We have a lot of work to do before it can be potentially translated into the clinic, but we feel confident that this is a very promising approach for bringing new hope to patients with glioblastoma so they can recover after surgery,” Hu says. “We hope we can do our work to be able to advance this technology to the clinic.
Although the approach caters to glioblastoma, in the future it can be used to treat other aggressive tumours, for example, breast cancer tumours.
Our approach is to take advantage of the macrophages in the postsurgical areas and to locally engineer these macrophages
Hu further added,
In this scenario, we can confidently say that it will apply to the majority of solid tumours with high invasive characteristics.