Case Presentation: History and Examination
A 44-year-old female from Kenya with HIV who was on anti-retroviral therapy for the past 14 years came to the OPD with the complaint of dry cough, sore throat, chest pain and muscle ache. She also complained reported vomiting 3 days prior to coming to the hospital, along with fever, chills, nausea, anorexia, and headaches.
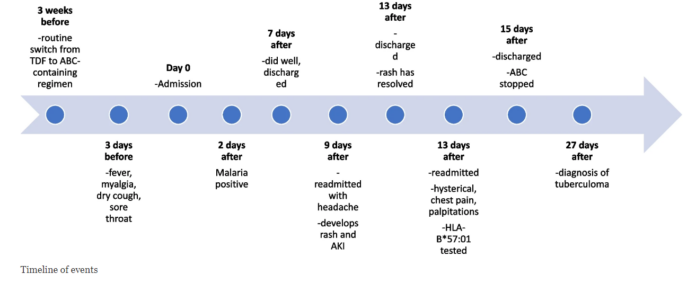
She told the doctors that her medications were switched to abacavir, lamivudine, and dolutegravir 3 weeks before. Additionally, previously, she was taking TDF, 3TC, and efavirenz but her medications were changed by her doctor as he deemed the new medications to be a better treatment regimen for her. She had been tested for malaria a couple of times, however, it always turned out negative.
Doctors did a throat examination, which showed inflammation with tender tonsils. Furthermore, her muscles were also tender to palpation. The rest of the examination was unremarkable with vitals that were stable. The doctors sent some baseline investigations which revealed a white cell count of 2.6 × 109/L (73% granulocytes, 22% lymphocytes), haemoglobin of 14.0 g/dL, and platelet count of 122 × 109/L.
Management
The doctors admitted her and commenced her treatment with intravenous rehydration and rest. The provisional diagnosis was a viral upper respiratory tract infection. Despite this management, her symptoms did not improve. She complained of a body ache on the second day in the hospital. The baseline investigations revealed an increase in liver enzymes. Therefore, the doctors ordered testing for hepatitis and malaria. She tested positive for malaria, and they started her management with artesunate.
Given her deranged liver function tests, the doctors suspended her anti-retroviral therapy. After the commencement of artesunate, her liver enzymes started to improve. Although, her muscle ache did not improve, and she complained of paresthesia and body swelling. The doctors discharged her on day seven when she started feeling better.
Re-admission with complications: Abacavir Hypersensitivity
She presented a day after discharge again with severe headache, profuse sweating, vomiting, diarrhoea, and lower abdominal pain. Her systemic examination was unremarkable. Doctors made a provisional diagnosis of hospital-acquired infection and started rabeprazole, antibiotics and ondansetron. Her baseline investigations revealed a creatinine of 183 µmol/L, which pointed towards acute kidney injury. Two days later she developed a rash on the extremities that spread to the trunk. Therefore, she was given cetirizine and mometasone cream. Her kidney function started to improve along with liver enzymes and the rash also improved. The doctors discharged her after 5 days.
However, the patient presented again on the night of the day of discharge, with chest pain and chills. Her systemic examination was normal with no rash on the body. The ABGs revealed respiratory alkalosis with elevated liver enzymes, LDH and potassium. Upon further questioning, the patient confessed to taking abacavir before she became unwell after which she vomited. Moreover, she revealed that she had been taking ART every time she was discharged, which was against the doctor’s recommendations.
The doctors commenced supportive management after she started improving. Although, peripheral neuropathy of the left lower limb did not improve. The doctors made a provisional diagnosis of abacavir hypersensitivity and ordered the HLA-B*57:01 test, which turned out positive. The doctors advised her to stop taking abacavir and discharged her after 2 days. She again presented 12 days later with headaches and confusion. A CT scan revealed parietal tuberculoma. The doctors started rifampicin, isoniazid, pyrazinamide, and ethambutol for 2 months, then rifampicin and isoniazid for 16 months, along with dexamethasone. Additionally, 2 months after this presentation, they changed her ART regimen to DTG and a fixed-dose combination of emtricitabine plus TDF.
This management regimen of ART and ATT stabilized her liver and kidney function tests. Although there was an overall improvement, her headaches persisted for 24 months after this treatment regimen.
Discussion: Abacavir Hypersensitivity
Abacavir hypersensitivity is a rare but fatal reaction to an HIV treatment regimen that occurs in 5% of these patients. It presents with a wide spectrum of clinical signs and symptoms. This can be avoided by testing patients for HLA-B*57:01 before commencing abacavir in HIV patients. However, this is not ideal in resource-limited hospitals and clinical setups. The underlying aetiology of abacavir hypersensitivity is controversial, although it is thought to arise from changes in the binding of abacavir to HLA-B*5701 peptides, which changes immunity and thus causes a hypersensitivity reaction.
Once this diagnosis was made, it is important to make the patient understand that they should not take abacavir as it can be fatal. Which in this case did not occur, as the patient did not stop taking the medication despite the doctor’s order.
The challenges highlighted in this case report faced by doctors in diagnosing the patient highlights the importance of HLA-B*5701 testing in such patients and also keeping a differential of this condition when assessing such patients.