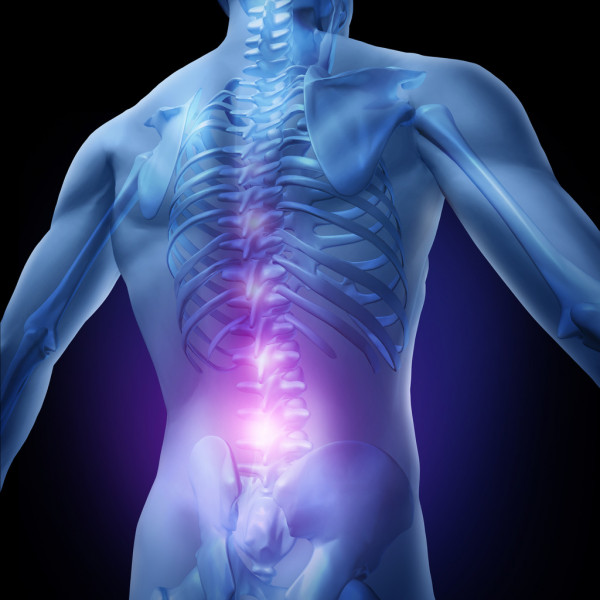
Using gene therapy, scientists at UC San Diego have developed a drug-free and safer solution for chronic pain.
Chronic pain affects 19 to 50% of the world’s population. Current treatments include opioids; however, they can cause adverse side-effects and pose a risk of addiction. Therefore, researchers are on the look for safer, non-addictive and long-lasting treatment options.
What we have right now does not work. There’s a desperate need for a treatment that’s effective, long-lasting and non-addictive
Ana Moreno, study author
Ana Moreno, a bioengineering alumna of UC San Diego, was working on her thesis when she came across a research paper describing a genetic mutation that caused people to not feel pain. The mutation inactivated NaV1.7, a protein involved in pain signalling between nerve cells. At the moment, Moreno was investigating a gene-editing technology called CRISPR for treating rare human diseases. She was working with a specific version of CRISPR that uses ”dead’ Cas9. This particular gene-editing tool can stick to a gene and block its expression but lacks the ability to cut DNA.
It’s not cutting out any genes, so there are no permanent changes to the genome. You wouldn’t want to permanently lose the ability to feel pain. One of the biggest concerns with CRISPR gene editing is off-target effects. Once you cut DNA, that’s it. You can’t go back. With dead Cas9, we’re not doing something irreversible.
Ana Moreno, study author
Thus, Moreno and her team began to engineer a CRISPR/dead Cas9 system that could target the gene coding for NaV1.7. They then injected these constructs into mice using spinal injections, while exposing them to inflammatory and chemotherapy-induced pain. The findings of the study are published in the journal Science Translational Medicine.

A Safer, Non-Addictive Alternate
The researchers assessed the mice at various time intervals. The results showed that the mice which received the injection had a higher pain threshold than those who did not. Overall, the treated mice had a lower sensitivity to pain. Moreover, the lasting effects were seen even after 44 weeks in mice with inflammatory pain, and 15 weeks in those with chemotherapy-induced pain.
To further validate their results, the researchers also performed the same lab study using another, older, gene editing tool called zinc finger proteins. It produced similar results. Thus, giving scientists an alternate that will likely not evoke an immune response in humans.
The long-lasting pain relief coupled with a lack of side-effects makes this a promising option for treating chronic pain. Study authors believe their treatment approach can help treat a range of chronic pain conditions along with providing relief in chemotherapy patients.
Reference:
Moreno, Ana M., et al. “Long-Lasting Analgesia via Targeted in Situ Repression of NaV1.7 in Mice.” Science Translational Medicine, vol. 13, no. 584, 2021, doi:10.1126/scitranslmed.aay9056.