Case Presentation
A 26-year-old Asian man was found shaking in the bathroom after ingesting Clorox and Dettol from two separate bottles. He was immediately brought to the ER where upon arrival, he was distressed, confused, and drooling. The emergency medical team gave him intravenous normal saline and oxygen to stabilize his vitals.
Upon inquiring, the patient complained of abdominal pain and a headache. The doctors checked his vital signs, which showed he was breathing at a rate of 22 breaths per minute. His oxygen saturation was 98% on a non-rebreather mask and his heart rate was 84 beats per minute. His blood pressure was high at 182/102 with a GCS of 13/15. Additionally, his oral mucosa and oropharynx were red, swollen, and had sloughed off tissue. Although he was drooling, he didn’t have stridor.
Due to the risk of airway compromise, the doctors intubated the patient. They put him on a mechanical ventilator in continuous mandatory ventilation (CMV) mode. They also obtained a blood sample to check his blood gases, blood count, urea and electrolytes, clotting screen, liver functions, and drug toxicology screen.
Investigations
The investigations revealed that his blood pH was lower than normal at 7.26. It had increased CO2 levels and decreased bicarbonate levels. He also had an increased level of lactate, indicating a buildup of waste products in his body. The patient had an elevated white blood cell count, indicating an infection or inflammation. He also had an abnormal blood clotting profile, suggesting liver compromise.
The patient’s liver function tests showed that he had elevated levels of AST and ALT. These are enzymes released by the liver when it is damaged. Additionally, his amylase and lipase levels were abnormally high, indicating pancreatitis. However, his toxicology screens for both urine and serum were negative.
A chest X-ray showed that the endotracheal tube was in the right position, but the patient had aspiration pneumonitis. A computed tomography (CT) scan of the head, neck, thorax, and abdomen revealed soft tissue swelling in the larynx and pharynx. Moreover, there were ground glass opacities in the right middle and lower lobes of the lungs. There was also evidence of contrast substance leakage in the stomach, peri-pancreatic and perigastric areas, and periportal oedema in the liver.
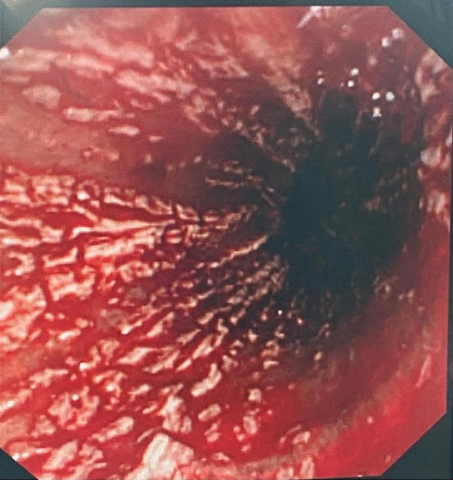
The doctors performed an esophagogastroduodenoscopy (OGD) on the patient, which revealed that he had severe erosive esophagitis. The doctors also found blood in the patient’s stomach with extensive haemorrhage. It led to difficulty visualizing the walls of the stomach and duodenum. Therefore, the doctors admitted the patient to the intensive care unit.
Prognosis
On the second day of admission, the patient had an abnormally high heart rate of 147 beats per minute and a low blood pressure of 76/55 mmHg. The results of repeated laboratory tests showed that the patient’s liver and kidney functions were worsening. Furthermore, his procalcitonin levels were high.
After the final analysis of the report of OGD, the doctors diagnosed the patient with gastrointestinal mucosa injury. This was caused by ingesting sodium hypochlorite and Dettol.
The patient’s laboratory test results showed that he had high levels of anion gap metabolic acidosis and hyperkalemia, which indicated that he was experiencing acute kidney injury. Therefore his organs, including his lungs, pancreas, and liver, began to fail, and he developed disseminated intravascular coagulopathy (DIC).
The doctors gave the patient a loading dose of intravenous pantoprazole at a strength of 80 mg, followed by a continuous infusion at a rate of 8 mg per hour. The doctors continued to administer intravenous normal saline to the patient. Moreover, they gave him intravenous piperacillin/tazobactam at a strength of 4 g/0.5 g. A catheter was inserted to monitor the patient’s urine output, and it was noted that the patient had frank hematuria (blood in the urine).
To treat the DIC, the doctors gave the patient recombinant factor VIIa, fresh frozen plasma, and cryoprecipitate. They also administered sodium bicarbonate and continuous renal replacement therapy. The doctors also gave him intravenous vancomycin for a wider range of antimicrobial coverage.
The patient’s blood pressure remained very low, therefore the doctors gave him norepinephrine, vasopressin, and packed red blood cell transfusions. The doctors transfused him with a total of 12 units of packed red blood cells, 23 packs of fresh frozen plasma, 3 packs of cryoprecipitate, and 3 units of platelets.
Conclusion
Despite receiving treatment, the patient’s metabolic acidosis and hyperlactatemia persisted. By the fifth day of hospital admission, the patient’s condition had not improved. The patient’s heart rate had slowed down significantly, and his blood pressure remained very low. The patient’s laboratory values also worsened, and the ICU multidisciplinary team decided to place a do not attempt resuscitation (DNAR) order. Unfortunately, the patient went into cardiac arrest and passed away.
Discussion
This case report discusses a rare and deadly outcome resulting from the ingestion of Dettol and sodium hypochlorite together. Dettol is a common household disinfectant that can cause mild symptoms like vomiting, throat pain, and dizziness if ingested in small amounts. However, ingestion of larger amounts can cause renal impairment and death. Similarly, sodium hypochlorite, the active ingredient in bleach, can cause cellular damage and even death if ingested in large quantities.
When these two products are combined, they can have additive effects on the body, especially on the gastrointestinal, renal, cardiac, and hepatic systems.
Patients with severe poisoning from products like Dettol and Clorox need continuous monitoring of vital signs, ECG, and blood gas analysis for at least 24 hours. If a patient has reduced consciousness levels or signs of upper respiratory tract obstruction, early intubation and airway protection should be done.
Renal impairment should be managed with intravenous sodium bicarbonate and early hemodialysis. A multidisciplinary approach involving gastroenterologists and otolaryngologists is essential for managing patients with Dettol poisoning.
Gastric lavage is not recommended due to the increased risk of aspiration. Upper gastrointestinal endoscopy should be done within 24 hours to determine the extent of the corrosive injury, but it is contraindicated in hemodynamically unstable patients or those with signs of perforation or airway compromise.
In conclusion, this case report emphasizes the importance of being cautious when using household disinfectants like Dettol and bleach, as ingestion of large amounts can have severe and potentially fatal consequences. If a patient does ingest these products, it is crucial to manage their symptoms and complications promptly and with a multidisciplinary approach.