Why is it important to highlight a case of fungal endophthalmitis?
Because untreated fungal endophthalmitis can lead to blindness.
Once a rare sight, the incidence of fungal endophthalmitis has increased in the past few years, particularly in the last two decades, especially in immunocompromised individuals.
Fungal endophthalmitis can be either endogenous or exogenous. In the latter, the causative fungus enters, most commonly, through trauma to the eye.
Below is an example of endogenous fungal endophthalmitis.
A 34-year-old man presents to the ophthalmology clinic with complaints of pain and decreased vision in his right eye for one week. He is an intravenous drug abuser and reports being a known case of hepatitis C.
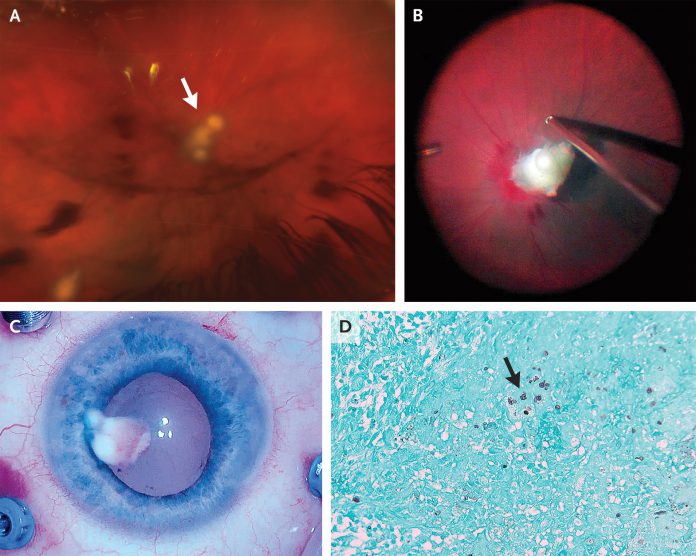
The visual acuity was 20/400 in the right eye. On the slit-lamp examination, the ophthalmologist noticed inflammation in the anterior chamber and conjunctival injection in the right eye. Indirect ophthalmoscopy revealed vitreous haze, and lesions on the retina and optic nerve (Panel A, arrow). The examination of the left eye was normal, along with the normal visual activity of 20/20.
Serological investigations were unremarkable with negative blood cultures.
Transthoracic echocardiography showed no evidence of vegetations, ruling out infective endocarditis secondary to IV drug use.
Fungal endophthalmitis was suspected
The patient was started on oral and intravitreal voriconazole (an antifungal). Despite being compliant with the treatment, the vitreous lesions didn’t resolve; therefore, vitrectomy was performed.
Intraoperatively, a white mass was incised and removed, which was adherent to the optic nerve. The mass measured 4 mm by 3 mm by 1 mm. Panel C shows the mass in the anterior chamber just before removal.
The incised mass was sent for histopathological evaluation. Gomori methenamine silver staining revealed a necrotizing granuloma with fungal yeast forms suggestive of candida species. (Panel D, arrow)
Postoperatively, his visual acuity improved to 20/30. Oral voriconazole treatment was continued for six weeks postoperatively.
At the 6-month follow-up, his vision was stable with no evidence of recurrence.
Although fungal endophthalmitis is a rare disease, recently, diagnosis of fungal ophthalmitis is surfacing more often than expected, probably due to advancements in the diagnostic modalities. Moreover, Candida species have seen to be predominating, and aspergillus is the second most common.
Symptoms vary according to the part of the eye affected. The causative fungus may cause vitritis, iritis, anterior uveitis, and endophthalmitis.
Why use Gomori methenamine silver stain?
Fungal organisms do not stain well on Gram
stain does not stain fungus well enough; therefore, Giemsa
or Gomori methenamine silver stain is used to spot fungal organisms.
Patients may lose vision due to fungal endophthalmitis.
Thus, early diagnosis and prompt treatment are required for a better prognosis. Otherwise, even after the treatment, the visual acuity may not improve.
References
John R. Chancellor, M. a. (2020, May 07). Fungal Endophthalmitis. Retrieved from The New England Journal of Medicine: https://www.nejm.org/doi/full/10.1056/NEJMicm1911882
Sridhar, Jayanth & Flynn, Harry & Kuriyan, Ajay & Miller, Darlene & Albini, Thomas. (2013). Endogenous fungal endophthalmitis: Risk factors, clinical features, and treatment outcomes in mold and yeast infections. Journal of ophthalmic inflammation and infection. 3. 60. 10.1186/1869-5760-3-60.