Vulvar squamous cell carcinoma with cutaneous and breast metastases.
This article describes the case of a 76-year-old female patient with cutaneous and breast metastases of vulvar cancer. The patient presented to the emergency department with a 3-week history of intense vaginal pain and bleeding. The patient’s medical history revealed coronary artery disease after artery bypass graft, aortic stenosis and hypertension. She had previously presented to the emergency 9 months ago because of mild vaginal itching and spotting.
For treatment, doctors initially prescribed her clotrimazole/betamethasone cream. However, the medication gave her a burning sensation. Therefore, doctors gave her topical oestrogen ointment with which her symptoms partially resolved. For further evaluation, a transvaginal ultrasound was performed which showed an endometrial strip of 5 mm. Although, no mass was seen. She was scheduled for a hysteroscopy with dilatation and curettage if the symptoms persisted.
The patient did not follow-up to the gynaecology clinic for 7 months till her visit to the emergency department.
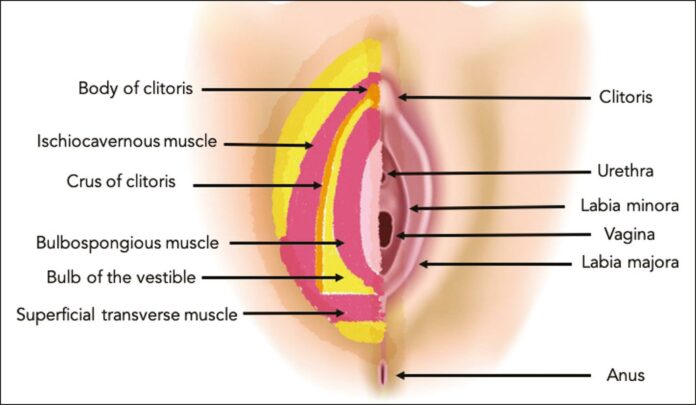
Her current pelvic exam showed a midline clitoral mass with foul-smelling discharge. Although, the examination was limited because of severe tenderness. The physical examination showed no other significant findings. The clitoral mass was examined under anaesthesia which showed that the mass encompassed the right and left labia. In addition, the mass was indurated and erythematous. Histopathological analysis of the mass confirmed the diagnosis of squamous cell carcinoma.
Doctors treated the patient with primary radiotherapy to vulva and pelvis considering the comborbidities and extent of disease.
She was on the treatment for the next 3 months. The patient reported improvement of vaginal pain at her 4 month follow-up after diagnosis. However, a rapidly growing mass, measuring 7 x 5 cm was palpable in her left upper back. The skin overlying the mass was intact and normal. PET CT showed metastases in the left inguinal lymph node, soft tissue lesion of left upper back and right breast. The immunophenotype profile suggested metastasis from vulva.
Doctors started her on carboplatin and paclitaxel chemotherapy. After receiving the first cycle of chemotherapy, her second cycle was delayed because she was admitted for pneumonia. The patient opted for hospice after she was discharged and died 9 months after her initial diagnosis.
References
Vulvar Cancer with Cutaneous and Breast Metastases https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7837761/