Adult direct Gerbode defect with an unusual diverticulated appearance
Gerbode defect is a defect in which the left ventricle (LV) communicates with the right atrium (RA). While initially the lesion was recognized as a congenital defect, it is now widely accepted as either an iatrogenic or non-iatrogenic origin. This article describes an unusual divericulated appearance of direct Gerbode defect in an adult patient. The patient did not have any history of cardiac pathology. In the Gerbode defect, the left ventricle (LV) communicates with the right atrium (RA).
Case report
A 46-year-old man with a 2-year history of fatigue presented with worsening shortness of breath. His medical history was significant for high blood pressure, though it showed no previous cardiac abnormalities. In addition, the patient was not diagnosed with any other metabolic syndrome. Additionally, he had no family history of congenital heart disease. Doctors further advised echocardiography and the findings were consistent with the diagnosis of Gerbode defect with a left-to-right shunt from LV to RA. The investigations were also significant for a diverticulated lesion around the area of Gerbode defect. This raised the suspicion of diverticulum that may have initiated the Gerbode defect.
Gerbode defect
Gerbode defect is a rare type of congenital heart defect that is a variant of ventricular septal defect (VSD). In this disease, there is communication between the left ventricle and the right atrium. The defect was first described by Thurnam in 1838. In addition, the defect was named after Frank Gerbode, a well-known surgeon from Stanford University. He published several cases of successful surgical repairs of patients with the condition in 1958. Isolated cases of the condition are rare and acquired lesion types are more common. The defect has iatrogenic, ineffective, traumatic or ischemic etiologies. However, the pathogenesis is still poorly understood for the congenital type. In some cases, NKX2-5, GATA4 and TBX5 have been implicated as gene sequence variations in some of the cases.
There are three different types of communication between the left ventricle and right atrium. Type 1 is indirect or infravalvular, type 2 is direct or supravalvular and type 3 is intermediate. Type 1 lesions are characterized by an intraventricular septal defect combined with a tricuspid valve defect. A direct connection between LV and RA is identified in type 2 lesions. Type 3 lesions are when there is a combination of both direct and indirect types of the gerbode defect. The global incidence of type 1 is 12%, type 2 is 81% and type 3 is 7%, respectively. This surgical case is an unusual presentation of the defect in an adult patient who has no prior history of cardiac pathology.
Case report
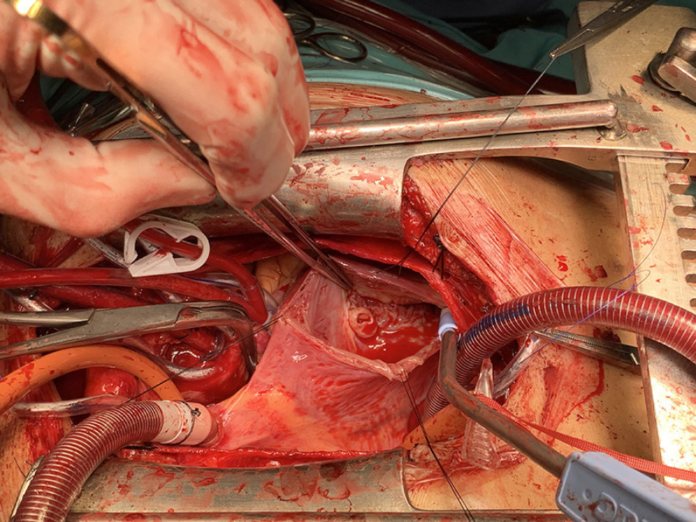
The author referred the patient for a median sternotomy. The procedure was done using a cardiopulmonary bypass, aortic cross-clamp and cold blood cardioplegia. The surgeons observed a septal defect upon opening the RA in the AV membranous septum. The lesion was diverticulated with a 1 cm opening and prominent blood flow that gushed from the left ventricle to the right atrium. The saline test further showed mild regurgitation and a flail at the edge of the tricuspid septal defect. “The Gerbode defect was closed using polytetrafluoroethylene (PTFE) patch with 9 circular pledget sutures. The TV was repaired using De Vega technique”.
The patient was transferred to the ICU after the surgery. There were no post-operative morbidities, for example, acute kidney injury, dysrhythmia or stroke. The patient was in the ICU for a day and then transferred to the immediate ward. Moreover, he did not require any urgent care. The patient was called back for a follow-up transthoracic echocardiography after 4 days of the procedure. He did not show any global wall motion normokinetics, residual tricuspid regurgitation, or residual VSD flow.



