Pleural effusion, a manifestation of chylothorax
This article describes the case of a rare presentation of neonatal chylothorax which led to respiratory distress in a neonate. The female infant was born at 25 weeks of gestation, via a vaginal breech delivery to a 36-year-old. The infant’s weight at the time of birth was recorded as 665 g. The mother’s medical history was consistent with pregnancy-induced hypertension. She was treated with nifedipine and antenatal steroids.
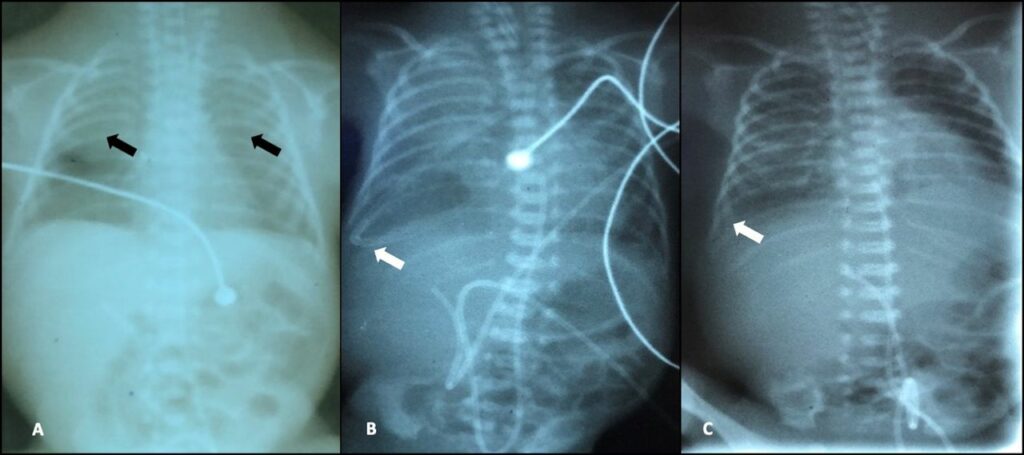
Neonatal chylothorax is a rare presentation which requires timely diagnosis because of its risk of respiratory distress. Chylothorax is an abnormal accumulation of fluid in the pleural space which causes respiratory and nutritional problems. It has a high mortality rate. Treatment includes resuscitation and the neonate is ventilated. Similarly, in this case, the infant had to be intubated soon after birth. While the patient improved clinically, the neonate developed subsequent respiratory distress and right-sided pleural effusion.
Neonatal chylothorax is a rare presentation which requires timely diagnosis because of its risk of respiratory distress
Treatment includes resuscitation and the neonate is ventilated. Similarly, in this case, the infant had to be intubated soon after birth. While the patient improved clinically, the neonate developed subsequent respiratory distress and right-sided pleural effusion. Doctors started the baby on trophic feeds and expressed breast milk (EBM) on the 2nd day. The feed was fully increased on the 5th day. However, because of an unavailability of custom preparations of parenteral nutrition required for managing the patient’s hyperglycaemia it was not introduced. Although the infant developed Coliform sepsis on the 3rd day, her respiratory-rate remained stable.
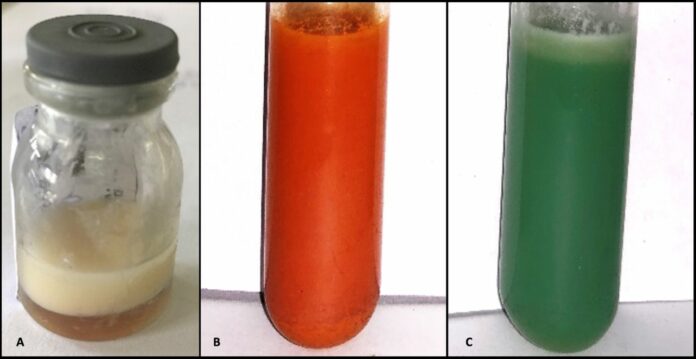
However, over days 9 and 10 the infant experienced a deterioration in the respiratory status. Doctors advised thoracentesis, a procedure for removal of fluid or air from around the lungs. Interestingly, the fluid had a milky appearance which led to the suspicion of chylothorax. Further investigations showed elevated levels of triglycerides and lymphocytes which confirmed the diagnosis of chylothorax.
A critically ill neonate generally presents with lower-than-average levels of fat leading to a reduced production of chylomicron, leading to lower triglyceride levels. Chylothorax is a diagnostic challenge because of a lack of age-specific triglyceride levels and low oral fat intake in neonates.
Source: BMJ



