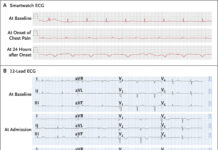
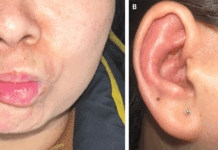
Malignant acanthosis nigricans in a 30-year-old woman
A 30-year-old woman presented with developing skin lesions on her face with a history three months presented to the dermatology clinic. Her lips, perioral region, and nasal folds all had hyperpigmented, yellow, papillomatous papules and plaques upon physical examination (Panel A). Her neck, inguinal areas, and axillae were similarly covered in hyperpigmented velvety plaques (Panel B). She also complained if fatigue, new-onset heartburn, and unexpected weight loss of 15 kg. A face lesion’s skin sample revealed epidermal papillomatosis, acanthosis, hyperkeratosis, and negative human papillomavirus staining. Malignant acanthosis nigricans was suspected to be the cause. A paraneoplastic dermopathy known as malignant acanthosis nigricans causes velvety plaques to appear suddenly on the cutaneous and mucosal surfaces.
Compared to benign acanthosis nigricans, the skin lesions are more extensive and worsen rapidly. On a computed tomography scan of the abdomen and pelvis, the right ovary had a solid mass measuring 4.4 cm in diameter, and the gastric body had thickened (Panel C, asterisks). The diagnosis of gastric adenocarcinoma with ovarian metastases, also known as a Krukenberg tumour, was confirmed by a gastric biopsy that revealed mucin-rich signet ring-cell adenocarcinoma. The cancer initially responded to systemic therapy, but by the 6-month follow-up, it had progressed.
Clinical presentation
The skin, in some cases, is the only clinical manifestation of cutaneous symptoms, which frequently signal an underlying disease. The invasion of the skin by a tumour or its metastasis are two examples of direct effects that can cause cutaneous manifestations of internal malignant tumours. Other indirect effects can result in cutaneous signs or symptoms that are associated with paraneoplastic syndromes.
Although it can affect any part of the body, acanthosis nigricans is a skin disorder marked by papillomatous, velvety, and hyperpigmented plaques that typically affect intertriginous and flexor areas symmetrically. There are two types of acanthosis nigricans: benign and malignant. According to Schwartz and Janniger (2011), benign acanthosis nigricans is linked to congenital anomalies, medication usage, and endocrinopathies like obesity, insulin resistance, diabetes mellitus 2, acromegaly, Cushing syndrome, and hypothyroidism. However, MAN is classified as a paraneoplastic dermatosis, i.e., it is associated to internal neoplasms but not a malignant illness in and of itself.
The condition was first described by Pollitzer and Janowsky
Pollitzer (1891) and Janowsky (1891) first described MAN in the same volume of the International Atlas of Rare Skin Diseases. It was later pointed by Darier that the condition is associated with internal malignancies which is consistent with the MAN being a paraneoplastic syndrome. Although the exact prevalence of this condition is unknown, it is more frequently seen in patients aged > 40 years. However, there is no gender predilection.
MAN can be defined as a sudden onset, progressive course and extensive condition. It is characterised by cutaneous and mucosal involvement. However, in some cases it may be associated with the development of acrochordons, multiple seborrheic ketatosis, oral papillomatosis and acanthosis nigricans palmoplantar. Studies have shown that 17.4% of the cases of MAN are diagnosed before the diagnosis of neoplasia. Whereas 61.1% and 21.5% are diagnosed during and after the diagnosis of neoplasia. Similarly, the skin lesions tend to improve with tumour resection. In addition, the occurrence of MAN has also been associated with a poor prognosis of cancer. On average, patients diagnosed with MAN survive <2 years after diagnosis.
Sources