Congenital Diaphragmatic Hernia
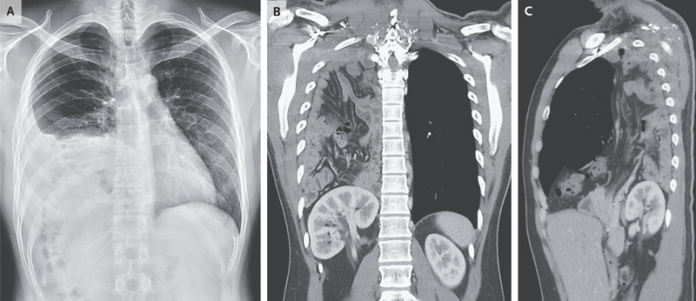
This article describes the case of a 25-year-old man who was referred to the emergency department because of abnormal results on the chest radiograph. Based on the investigation findings, the doctors diagnosed the patient with a congenital diaphragmatic hernia. The patient was undergoing a pre-employment examination and had no known medical history or symptoms. The patient’s respiratory rate was 14 breaths per minute and oxygen saturation was 100% while breathing ambient air. The examination further showed decreased breath sounds at the base of the right lung. The examination further showed a non-tender abdomen. Doctors further advised a chest radiograph which was significant for pleural effusion, a suspected translocation of the colon into the right upper quadrant of the abdomen and an elevated right hemidiaphragm.
The patient was further referred for computed tomography of the chest with contrast material which showed herniation of the right kidney, and small and large intestines into the right thoracic cavity through a posterolateral diaphragmatic defect and omentum. Based on these findings, the patient was diagnosed with a congenital diaphragmatic hernia, secondary to a posterolateral diaphragmatic defect. The condition is also referred to as Bochdalek hernia. Doctors advised surgical repair, however, the patient declined and was also lost to follow-up [1].
Bochdalek hernia
While Bochdalek hernia is typically diagnosed in infants and children with the presentation of respiratory distress, in rare cases, it may remain asymptomatic until adulthood. It often presents with complications of bowel strangulation or obstruction during adulthood, as with this case. Congenital diaphragmatic hernia is a relatively common idiopathic malformation that presents during the newborn period. The condition is known to occur in five babies per 1000 births. Studies have shown that it is slightly more frequent in men and less common in Blacks [2]. The disease is generally detected via ultrasonography screening during fetal life. The ultrasound is significant for herniation of the bowel or the liver into the thorax which allows a correct pre-natal diagnosis in 50 to 90 percent of the cases.
In some severe cases, polyhydramnios may lead to an antenatal diagnosis. Congenital diaphragmatic hernia is common because of respiratory distress or gastrointestinal disease due to obstruction and incarceration of herniated bowel loops. It is further seen that persistent pulmonary hypertension and pulmonary hypoplasia may lead to respiratory insufficiency. The cause of pulmonary anomalies is often linked with intra-thoracic compression of the lungs by the herniated abdominal viscera which may lead to an alteration of pulmonary blood flow.
Late presentation of CDH is difficult to diagnose and may cause delays in treatment. All diaphragmatic defects can be closed without any post-operative complications using an abdominal approach. CDH in adults generally presents with gastrointestinal tract symptoms, such as vomiting, intermittent abdominal pain and dysphagia. Respiratory symptoms may include dyspnoea and chest pain. Similarly, depending on the herniation of the abdominal viscera into the thorax, symptoms are either intermittent or acute. The acute presentation is generally because of incarceration, strangulation of the herniated viscera or obstruction. The diagnostic tools for CDH include a combination of X-rays, CT and magnetic resonance imaging (MRI). Diagnosis may also be done using upper GI and bowel-contrast studies.
Investigation findings and management
CDH is characterised by the abutment of fat or soft tissue along the upper surface of the diaphragm on a CT scan, generally along the upper surface of the diaphragm or posterolateral to the hemidiaphragm. Other findings may include diaphragmatic discontinuity adjacent to the mass and continuous density above and below the diaphragm through the defect. Bochdalek hernia in some cases may also be misdiagnosed as pleural effusion, atelectasis, lung cysts, tension pneumothorax and pneumonia. Pneumonia or pneumothorax can be ruled out by placing a feeding tube and instillation of contrast material.
In addition, incorrect diagnosis and a delay in treatment can be avoided with a careful analysis of the chest films and with a thorough search for connecting bowel segments passing through the defect. The hernia is managed by reducing abdominal contents and repairing the defect via a laparotomy or thoracotomy. A thoracic or thoracoabdominal approach usually deals with right-sided defects because of the presence of the liver. Whereas, in case of left-sided hernias a transthoracic approach or a transperitoneal approach is suggested.
References
- Liu, H.H. and Liu, Y.C., 2022. Congenital Diaphragmatic Hernia in an Adult. New England Journal of Medicine, 386(16), p.e42.
- Bianchi, E., Mancini, P., De Vito, S., Pompili, E., Taurone, S., Guerrisi, I., Guerrisi, A., D’Andrea, V., Cantisani, V. and Artico, M., 2013. Congenital asymptomatic diaphragmatic hernias in adults: a case series. Journal of medical case reports, 7(1), pp.1-8.



