This article describes the case of a patient with a Bone Marrow Transplant (BMT) who developed unusual ophthalmological complications.
A 19-year-old boy presented to the hospital, four months after undergoing BMT for his acute lymphoblastic leukaemia (ALL). When presented, he only complained of bilaterally decreased vision and fever for 2 days. He did not report any pain or photophobia or any problems in the perception of images in the context of size and shape.
The patient was taking cyclosporine to prevent transplant rejection. Moreover, his prescription included prophylactic antifungal and antiviral medication. He also revealed undergoing whole-body irradiation and chemotherapy to treat ALL.
Examination Reveals Retinopathy
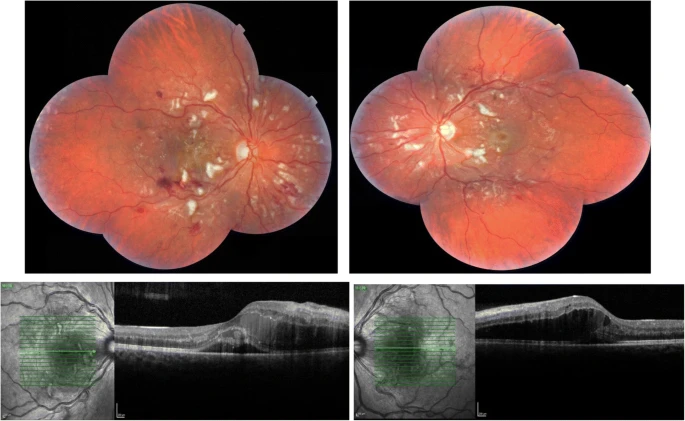
The patient was admitted to the haematology department. He showed low haemoglobin levels and the doctors could not work out a cause for his pyrexia. On examination, he displayed decreased visual acuity in both eyes, more in the right eye. Fundoscopy revealed retinopathy in both eyes with cotton wool spots and retinal haemorrhages. Additionally in the right eye, doctors also found fluid in the sub-retinal space on optical coherence tomography (OCT) suggesting a possible retinal detachment. Overall, the central retina was more affected while the peripheral retina was spared.
Management and Outcome of the Patient
On the account of patient’s retinal pathologies and pyrexia, doctors performed an anterior chamber tap. They sent the tapped fluid for culture and it turned out negative for any viral colonies ruling out viral retinitis. The absence of infection now suggested cyclosporine as the likely cause of visual disturbances because cyclosporine is retinotoxic. Thus, doctors stopped cyclosporine and started the patient on oral steroids instead.
Over the subsequent days, the patient’s visual acuity improved and a little later, his macular oedema started resolving too. However, the patient could not achieve haematological stabilization. His systemic health became more and more compromised and he eventually died of pulmonary complications.
BMT and Retinopathy: What Are the Odds?
Bone marrow transplant, just like any other transplant procedure, comes with its own risks and benefits. Still, for patients with acute lymphoblastic leukaemia who do not respond to anticancer drugs, it remains the treatment of choice.
BMT is known to cause ocular complications. However most of the time, the complications occur as a result of cyclosporine that is given to the patient to prevent transplant rejection. The other common cause remains an infection. Whatever the cause may be, the complications usually occur in the anterior part of the eye involving the sclera or choroid such as keratoconjunctivitis. Posterior segment diseases or retinopathies occur only rarely.
Pathogenesis and Prognosis
Retinal pathologies develop as a result of changes in the microvasculature of the retina. Either hypertension or ischemia sets off a series of changes that ultimately lead to the deterioration of vision.
In the case of retinal ischemia, the release of vascular endothelial growth factor causes the development of new vessels (neovascularization) first at the optic disc and then elsewhere. These new vessels are thin and fragile and thus leak very easily. Leakage from these vessels causes retinal haemorrhages. Moreover, the remains of these vessels get replaced by fibrotic bands that exert traction and cause retinal detachment.
Hypertensive retinopathy shares a similar pathogenesis. High blood pressure in the retinal microvasculature leads to haemorrhages in both the superficial and deeper layers of the retina. The resulting haemorrhages are called flame-shaped haemorrhages and they too significantly deteriorate vision.
BMT and Retinopathy: The Bottom Line
Along with a lot of other complications associated with organ transplantation such as transplant rejection and hypersensitivity reactions, bone marrow transplantation causes ocular complications too. However, most of these complications involve the anterior segment of the eye. This case describes a rare occurrence of retinopathy with findings such as retinal haemorrhages and retinal detachment post-bone marrow transplant. Moreover, it also highlights that if early intervention is done, the defects in visual acuity and macular oedema can be reversed.



