A radioiodine therapy done for hyperthyroidism showed its side effects 14 years after the procedure!
A 60-year-old Chinese woman was brought to the hospital by her daughter with complaints of altered mental status for the past 1 week after her mother fell. The daughter explained that since the fall, her mother had been agitated, withdrawn, and had an auditory hallucination of her children asking her to meet them at a café and a visual hallucination of a doctor pressing the call bell. All these symptoms began only after the fall; otherwise, she was completely fine before the fall and never had any of these symptoms. The patient was previously able to perform activities of daily life, including housework and grocery shopping. There was no history of any psychiatric condition in her or her family, neither the patient had a history of substance abuse.
On physical examination, no remarkable findings were noticed. Serological investigations revealed normocytic, normochromic anemia, normal liver enzymes, no electrolyte abnormalities, and normal renal function. Urinalysis was also normal, and no drugs were found in her urine sample.
Imaging studies were conducted to look for consequences of the fall, but computed tomography of the brain showed no intracranial bleed or skull fracture. An MRI of the brain was performed, which was also unremarkable without any signs of intracranial bleed or infarction.
The chest X-ray was also unremarkable.
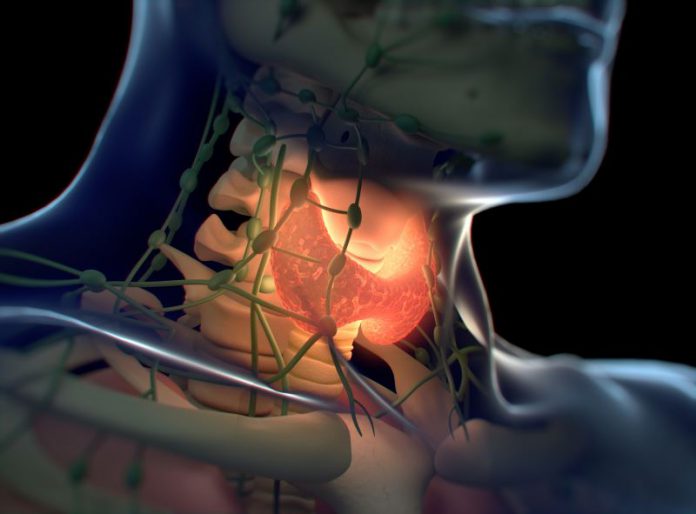
Further investigations revealed primary hypothyroidism. Upon inquiring the patient’s daughter about her mother’s thyroid disorder history, she revealed that her mother had received radioiodine therapy for hyperthyroidism 14 years ago; since then, the patient had neither taken any thyroxine replacement nor had any follow-up.
The daughter showed a thyroid function test report from 14 years back, which was the latest available test. The report showed primary hypothyroidism with the following values:
- Free thyroxine 9.2 pmol/l (9.6–19.1)
- Thyroid-stimulating hormone (TSH) 38.7 mU/l (0.36–3.25)
The daughter denied any hypothyroid symptoms in her mother.
A working diagnosis of psychosis with delusions, thought disorder, and hallucinations was made. The patient was started on olanzapine (antipsychotic) and lorazepam (benzodiazepine) and she was also given levothyroxine at a dose of 25 µg daily. The dose of levothyroxine was increased to 50 µg daily after 3 days.
Within one week of initiating treatment, the patient improved substantially, and her psychotic symptoms had also resolved.
The patient was discharged after she was stabilized with a prescription of olanzapine and thyroxine.
Two weeks after her discharge, she was reviewed by the same treating psychiatrist who was told that she was taking levothyroxine regularly but had not taken even a single dose of olanzapine. The patient had no episode of psychosis.
The patient was diagnosed to have radioiodine-induced hypothyroid psychosis.
At the 2-month follow-up, the patient had no complaints, nor she had any episode of psychosis despite not taking antipsychotics.
She was discharged from the psychiatrist’s follow-up with advice to take levothyroxine regularly.