Case Presentation:
A 47-year-old Middle Eastern woman presented to the King Hussein Cancer Center in September 2022 for further treatment of her breast cancer, which had spread to other parts of her body. She had been diagnosed with breast cancer and had received initial treatment at different hospitals over the course of her illness.
History
The patient did not give any history of smoking or drinking alcohol. Although, she was diagnosed with a heart condition called supraventricular tachycardia, for which she was taking bisoprolol. She was married with two sons and a daughter. Before coming to the King Hussein Cancer Center, she didn’t have any mental health problems. However, during her hospital stay, she experienced major depressive disorder, with symptoms such as feeling sad, having a decreased appetite, feeling tired and weak, and losing interest in things she used to enjoy. She didn’t have any suicidal thoughts. Moreover, she had never taken any antidepressant or antipsychotic medications before.
Breast Cancer Diagnosis
In 2017, doctors diagnosed her with stage III invasive ductal carcinoma in her left breast. There was no metastasis at that time, according to the radiological investigation. The tumour biopsy showed that the cancer cells had estrogen receptors (ER) and a small percentage had progesterone receptors (PR), but there was no human epidermal growth factor receptor 2 (HER-2/neu). She underwent a modified radical mastectomy and then received 25 sessions of radiation therapy to the left breast. She also took tamoxifen as a hormonal therapy until 2020.
However, soon after, further imaging revealed that the cancer had spread to her left axillary lymph nodes, spine, ribs, liver, and both lungs. Doctors then treated her with paclitaxel-fulvestrant-letrozole. After treatment for the metastasis, a follow-up imaging showed that the known metastases had progressed further. So, in February 2021, doctors changed her treatment to gemcitabine-carboplatin and alpelisib.
In 2021, the patient developed severe back pain, which also radiated to her left thigh. An MRI of her spine showed that the cancer had spread to multiple locations. She received several sessions of external beam radiotherapy to help relieve the pain. Later on, she underwent palliative chemotherapy using vinorelbine-capecitabine, but the disease continued to progress. She did not use scalp cooling during her chemotherapy treatments. Her last chemotherapy session took place on June 5, 2022.
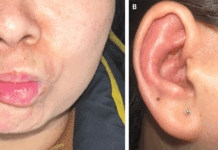
Scalp Metastasis
On September 15, 2022, the patient presented to King Hussein Cancer Center hoping to great treated with new chemotherapy options but she was not eligible for them. Her presenting complaint was the growing scalp nodules for the past 2 months. They were itchy, slightly painful, and had been rapidly increasing in size, especially in the three weeks before her visit. During the physical examination, doctors found three nodules on her scalp. The largest one, measuring approximately 4 cm × 3 cm × 0.5 cm, was located on the left frontal area. The other two were in the left parietal region, measuring around 20 mm × 10 mm × 5 mm and a few millimetres, respectively. The nodules were red, firm, immobile, and not tender. The surface was uneven, but there was no discharge on palpation.
Brain MRI revealed three scalp lesions. On September 15, 2022, doctors performed a punch biopsy on the largest scalp nodule. The biopsy results indicated metastatic invasive ductal carcinoma with positive estrogen receptors (ER) (95%), progesterone receptors (PR) (5%), cytokeratin-7 (CK-7), and GATA binding protein 3 (GATA-3). P63 and KIT (CD117) were negative in the tumour cells, and the score for human epidermal growth factor receptor 2 (HER-2/neu) was zero. The doctors did not give the patient any treatment for the scalp metastases due to a chest infection and bilateral malignant pleural effusion, which were confirmed by cytology. Unfortunately, her condition progressed to septic shock, and she passed away in the hospital.
Discussion: Breast Cancer Metastasis
Approximately 6% of women diagnosed with breast cancer will have metastatic lesions. These metastases can occur through different routes, such as the bloodstream, lymphatic system, or by spreading directly from the primary tumour.
The most common sites where breast cancer spreads are the lungs, bones, liver, and brain. Although skin metastases from breast cancer are rare, they can affect about 25% of breast cancer patients, usually appearing after the initial cancer diagnosis.
Metastases to the scalp are uncommon and account for only 2% of all skin tumours. However, the scalp region itself represents around 4-6.9% of all cases of skin metastases, likely due to its rich blood supply. Scalp metastases indicate disease progression and often have a poor prognosis.
Differentiating skin metastatic breast cancer from other types of tumours requires a histological examination. A primary skin adnexal adenocarcinoma, which originates from sweat glands, is the main differential diagnosis. Since the treatment and prognosis for these two types of tumours differ greatly, it’s crucial to obtain a definitive diagnosis.
Markers such as estrogen receptors (ER), cytokeratin-7 (CK-7), GATA binding protein 3 (GATA-3), and p63 can help distinguish between breast carcinoma and cutaneous adnexal tumours. However, no single marker is diagnostic, so a combination of markers should be used.
Conclusion
In conclusion, metastatic breast cancer can manifest in the skin, including the scalp, and careful histological examination is needed to differentiate it from other skin tumours. Scalp metastases can be an indication of disease progression, and the prognosis is often poor. The use of multiple markers is necessary for accurate diagnosis, and scalp cooling during chemotherapy does not increase the risk of scalp metastasis. To confirm the diagnosis and differentiate them from skin tumours, a biopsy with immunohistochemical (IHC) tests is necessary. Depending on the results, doctors adjust the treatment plan, such as using topical chemotherapy or performing local surgery, depending on the patient’s condition.