Case Presentation
An Iranian 14-year-old boy, without any previous medical history, presented to the hospital emergency. He had suffered severe injuries and had a deep cut on his right knee and a star-shaped cut on his head. Although his vital signs were stable, his oxygen saturation level was 93% and his temperature was high at 38.5°C. His Glasgow Coma Scale (GCS) score was 3/15. During his stay in the hospital, the boy tested positive for COVID-19.
Investigations
Doctors performed a focused assessment with sonography (FAST) for trauma which revealed that there was no free fluid in his abdomen or pelvic cavity. Additionally, his electrocardiogram showed a right bundle branch block. Despite a regular echocardiogram report, doctors admitted him to the neurosurgery ward.
During his stay in the hospital, doctors performed a high-resolution computed tomography (HRCT) scan of his lungs without contrast. This scan demonstrated patchy ground-glass opacity in both lungs (mostly in the right lung). The results suggested that he was infected with COVID-19. Subsequently, doctors performed a COVID-19-reverse transcription polymerase chain reaction (RT-PCR) test which confirmed the presence of the infection.
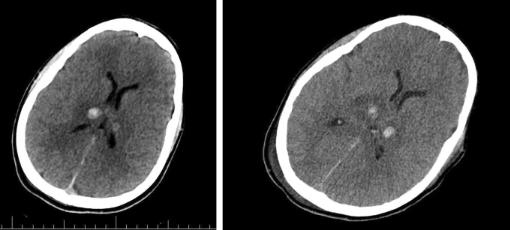
Moreover, doctors conducted a CT scan of the brain, which revealed a deep intracranial haemorrhage in the thalamus. Additionally, a contusion in the right parietal lobe was reported, however, there were no signs of hydrocephalus or shift in the midline brain structures. The CT scan of the cervical spine revealed no fractures or dislocations. The abdominal and pelvic CT scans were also normal.
Management
Doctors performed surgery for the laceration on the boy’s head. They also treated his knee laceration. They intubated the patient along with a cervical spine collar. To help lower the pressure in his brain, doctors gave him furosemide and mannitol. He stayed in the hospital for 40 days. On discharge, the doctors briefed his parents on how to take care of him. At the time of his discharge, his Glasgow Coma Scale (GCS) score was 6/15.
Discussion
This report highlights the case of a 14-year-old boy who was brought to the emergency room after sustaining multiple injuries. He did not have a history of any blood clotting disorders or a history of taking anticoagulants. Due to the injuries, he suffered a brain contusion and bilateral basal ganglia haemorrhage. Thus the diagnosis of ischemic stroke secondary to COVID-19 was the most probable cause.
Doctors ruled out trauma as the cause of these findings due to the rarity of basal ganglia haemorrhage secondary to traumatic events. These regions are most commonly affected by systemic and metabolic diseases, neurodegenerative diseases, and vascular diseases.
Covid-19 associated neurological complications
COVID-19, like other respiratory syndromes, can spread to the central nervous system via hematogenous and neuronal spread. Additionally, COVID-19 can trigger cytokines, which can also affect the neurological system.
Although the underlying mechanisms behind neurological disorders caused by COVID-19 are not fully understood, data suggests that around 2% of patients experience neurological symptoms. One of the ways COVID-19 can invade the neurological system is by infecting the olfactory receptor cells in the nose. This causes viruses and infections to be transmitted to the brain through the olfactory nerves.
Ischemic stroke can be a complication of COVID-19. Some of the underlying causes of this condition in COVID-19 patients include reduced blood flow to the brain, hypertension that can lead to posterior reversible encephalopathy syndrome, and septic embolization associated with bacterial superinfections.
The angiotensin-converting enzyme-2 (ACE-2) protein plays an important role in various parts of the body, including the lungs, kidneys, brain, liver, and endothelial cells. The virus reduces the expression of ACE2, which can cause damage to multiple organs. In the brain, low levels of ACE2 can lead to intracerebral haemorrhage through various mechanisms, such as increased blood pressure, endothelial dysfunction, damaging brain vessels, and depressing angiotensin-(1-7) and Mas receptor signalling. This signalling has a protective effect on the brain, through its antifibrotic and vasodilatory action.
It’s important to note that while there have been cases of COVID-19-related intracerebral haemorrhage, more research is needed to understand the association between COVID-19 stroke. However, it’s clear that reducing the risk of developing COVID-19 through vaccination and practising preventative measures such as wearing masks and practising social distancing can help decrease the risk of developing serious complications, including ischemic stroke.
There is a theory that a state of hyperinflammation in people with diabetes and COVID-19 could be the main cause of complications and higher mortality rates. High levels of a protein called C-reactive protein (CRP) can increase the risk of stroke and intracranial haemorrhage in COVID-19 patients.
Conclusion: COVID-19
Understanding the underlying mechanisms of neurological symptoms caused by COVID-19 is crucial. These symptoms can range from mild, like headaches, to severe, like strokes. It is important to identify the causes and methods of preventing these severe conditions to improve the prognosis of patients diagnosed with COVID-19.