Rare case of multiple aortic thrombosis
Venous thromboembolism is a common and well-recognised complication of COVID-19 disease. Whereas cases of arterial thrombosis are also increasingly reported, manifesting as stroke and myocardial infarction. In a similar case a 56-year-old female patient presented to the hospital after a fall with a 2-day history of worsening dyspnea. The patient’s medical history revealed postherpetic neuralgia, vitamin D deficiency, iron deficiency anaemia, major depression and hypothyroidism. She also complained of a 7-day history of fever and malaise.
Examination showed that the patient was tachpnoeic, febrile and hypoxemic. Doctors advised a chest X-ray and a test for COVID-19 on real-time PCR assay. X-ray showed multiolobar ground glass infiltrates and the patient was positive for COVID-19. A CT scan of the head and cervical spine was also performed because of her recent falls. However, findings of the CT scan were unremarkable.
Aortic thrombosis is a common complication of COVID-19 infection.
Although less frequent than arterial thrombosis, COVID-19 infection is associated with an increased risk of venous thromboembolism. The incidence of arterial thrombosis in critically ill patients is 4.4%, most commonly occurring in the extremities and cerebral vessels. Whereas the involvement of great vessels is around 19% in all the cases associated with COVID-19.
Other documented risk factors of COVID-19 include, chronic kidney disease, atrial fibrillation, hypertension and diabetes mellitus. Ascending aortic thrombosis is rare because of blood flow and higher pressures associated with embolic phenomena.
The patient was treated with remedesivir and dexamethasone for COVID-19 and for secondary bacterial infection coverage, ceftriaxone.
She eventually required orotracheal intubation because of progressive hypoxemia and delirium. Further laboratory tests were remarkable of “elevated D-dimer of 1.58 µg/mL with normal platelet count of 304×109/µL and prothrombin time was 11 s, stable low haemoglobin level of 95 g/L”. Peripheral smear was negative for schistocytes, ruling out the diagnosis of disseminated intravascular coagulation. Pulses were palpable in all four extremities of the patient with no signs of oedema.
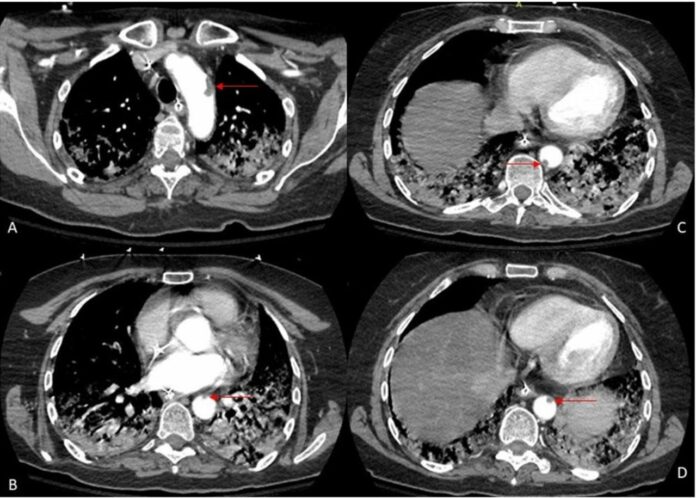
Doppler results of the lower extremities were negative for venous thrombosis. Doctors further advised a CT angiogram of the chest after the patient was stable. The results showed no signs of pulmonary embolism in the arch of the aorta and descending thoracic arch. CT scan of the head showed no large ischaemic thromboembolic strokes. ECG was consistent with sinus tachycardia. Echocardiogram findings were also unremarkable.
There was no need for surgical interventions because there was no development of any overt arterial or venous thromboembolic events. The patient was discharged on anticoagulation therapy and was advised for follow-up after 6 months of anticoagulation.
References
A rare case of multiple aortic thromboses associated with severe COVID-19 infection https://casereports.bmj.com/content/14/5/e242196



