Immunity is a barrier between humans and pathogens. Any breach in this protective barrier can lead to deadly infections by the same pathogens that would have caused a localized infection/no infection had the individual been immunocompetent.
An 8-year-old boy, known case of B-cell leukemia, presented to the outpatient department with a one-week history of subcutaneous nodules and fever. The patient had been started on treatment for a relapse of B-cell leukemia 2 months back.
He had pancytopenia for 57 days, and complete blood count showed the following results:
Hemoglobin level – 7.5 g per deciliter (reference range, 11.5 to 14.5)
White-cell count – 200 per cubic millimeter (reference range, 5000 to 11,000)
Platelet count – 12,000 per cubic millimeter (reference range, 150,000 to 400,000).
The subcutaneous nodules developed after 1 week of treatment with intravenous broad-spectrum antibiotics and antifungals. Also, the fever did not resolve despite treatment.
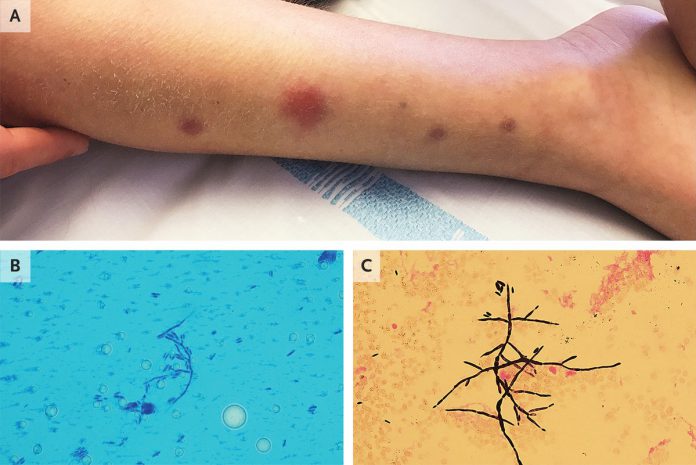
On examination, nodules ranging from 5 to 18 mm in diameter were seen on the arms, legs, chest, and back (Panel A).
A sample was obtained from the nodule. Septated hyphae and spores were seen on the microscopic examination of a dry smear when stained with lactophenol cotton blue (Panel B). Blood culture also revealed hyphae and spores on gram staining(Panel C).
The culture of the specimen and the blood, both grew Fusarium dimerum.
Antifungal therapy was initiated. The fever took 11 days to subside, and the nodules resolved within 20 days.
Fusarium species can cause superficial, localized, or disseminated infections, depending upon the host factors and the specie of Fusarium.
Immunocompromised individuals, such as the patient in the discussion here, with hematological malignancies, are prone to serious widespread infections by pathogens that otherwise cause localized infections. Similarly, disseminated fusariosis exclusively occurs in immunocompromised patients.
Such invasive fungal infections are one of the leading causes of mortality and morbidity in immunocompromised patients.
Patients with pancytopenia or neutropenia with disseminated fusariosis may present with fever, fatigue, myalgias (muscle aches), and skin lesions, i.e., painful nodules with central ulceration, that develop typically on the trunk, arms, and legs.

Image Source: NCBI
It is imperative to diagnose it early in the course, as the infection can spread rapidly and may get fatal if left untreated. Suspected cutaneous lesions in immunocompromised individuals require prompt histopathological evaluation and cultures. Also, Fusarium can be isolated from blood cultures.
Histopathological results show branching hyaline septate hyphae. It should be followed by culture to identify the pathogen as Fusarium cannot be isolated and diagnosed on histopathology only.
Early diagnosis and management are vital to reduce the associated mortality and to improve the prophylaxis. Immunosuppressed patients should be given prophylaxis with antifungals to prevent disseminated/invasive fusariosis.
However, treatment includes systemic antifungals, management of the underlying disease (such as management of the hematological malignancy), and surgical debridement of the infected sites.
Voriconazole, Posaconazole, and Amphotericin B can be used, either in combination or as monotherapy. The efficacy of mono- or combined therapy is yet under research. However, prophylaxis and earlier treatment for a prolonged period is the key to a better prognosis.
References:
Jacques Sevestre, a. L. (2020, May 21). Disseminated Fusariosis. Retrieved from The New England Journal of Medicine: https://www.nejm.org/doi/full/10.1056/NEJMicm1911084
Muhammed M, Anagnostou T, Desalermos A, Kourkoumpetis TK, Carneiro HA, Glavis-Bloom J, et al. Fusarium infection: report of 26 cases and review of 97 cases from the literature. Medicine (Baltimore). 2013;92:305-16.
Varon AG, Nouér SA, Barreiros G, Trope BM, Akiti T, Nucci M. Antimold Prophylaxis May Reduce the Risk of Invasive Fusariosis in Hematologic Patients with Superficial Skin Lesions with Positive Culture for Fusarium. Antimicrob Agents Chemother. 2016;60:7290-4.