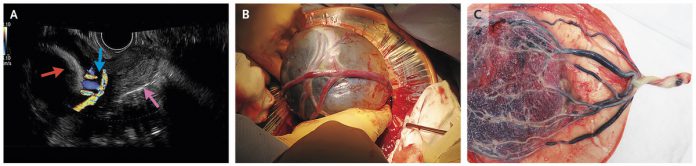
A 37-year-old pregnant woman at 27 weeks of gestation presented to the obstetrical clinic for her routine prenatal visit. She had no active complaints. Transvaginal ultrasonography (TVS) showed a low-lying posterior placenta (normally the placenta is anterior and away from the os) and velamentous cord insertion.
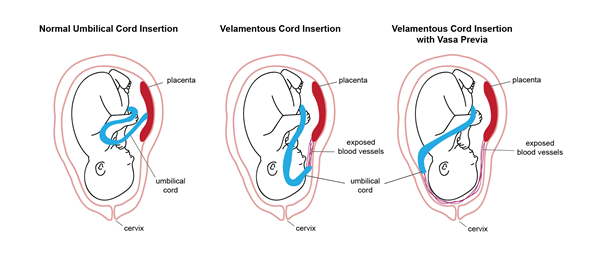
Velamentous cord insertion is a complication where the umbilical cord inserts onto the chorioamniotic membrane (fetal surface) rather than the placenta. Normally, 99% of the time, the umbilical cord inserts onto the mid of the placenta; in 1% of the pregnancies, the umbilical vessels, on their way to the placenta, diverge while traversing the chorioamniotic membranes.
The mother underwent transvaginal color Doppler ultrasonography, which showed that the internal os of the cervix is covered by the traversing fetal blood, a finding consistent with vasa previa.
An elective cesarean section with a low, transverse incision was performed at 34 weeks of gestation, which revealed fetal blood vessels crossing over the intact amniotic membrane that covered the head of the fetus (Panel B).
Examination of the placenta revealed membranous vessels that merged to form the umbilical cord, confirming the presence of velamentous cord insertion (Panel C).
The intrapartum course was uncomplicated; however, the neonate had transient tachypnea of the newborn but recovered completely afterward. There were no other complications, so both mother and baby were discharged soon after.
In vasa previa, the fetal vessels are around 2 cm from the internal os of the cervix or over the os, unprotected by the Wharton’s jelly, thus prone to compression and rupture during vaginal delivery and labor.
The most common presentation is painless vaginal bleeding at the time of labor when the membrane rupture or after amniotomy. The blood loss is primarily from the fetal vessels; therefore, it is fatal for the baby. Bleeding due to vasa previa causes abnormal fetal heart tracing and increased risk of fetal mortality.
If diagnosed earlier, it is best to plan elective cesarean section between 34 to 36 weeks of gestation to avoid complications as vasa previa is associated with adverse perinatal outcomes.
REFERENCES:
Shinya Matsuzaki, M. P. (2019, January 17). Vasa Previa. Retrieved from The New England Journal of Medicine: https://www.nejm.org/doi/full/10.1056/NEJMicm1808778
Rocha J, Carvalho J, Costa F, Meireles I, do Carmo O. Velamentous cord insertion in a singleton pregnancy: an obscure cause of emergency cesarean-a case report. Case Rep Obstet Gynecol. 2012;2012:308206. doi:10.1155/2012/308206